Thoracic Outlet Syndrome and Acupuncture Treatment
Thoracic Outlet Syndrome (TOS) is a complex condition characterized by the compression of nerves, arteries, or veins in the thoracic outlet, the narrow space between the collarbone and the first rib. This compression can lead to a range of symptoms, including pain, numbness, and weakness in the upper extremities. Affecting individuals of all ages, TOS can significantly impact daily life if not addressed properly. While conventional treatments like physical therapy and surgery are common, acupuncture has emerged as a promising complementary therapy for managing TOS symptoms. This article provides an in-depth exploration of TOS, including its definition, causes, symptoms, and conventional treatments, while focusing on acupuncture’s role in treatment, key acupoints, and its integration into a holistic care plan.
- What Is Thoracic Outlet Syndrome?
- Prevalence and Risk Factors
- Symptoms of Thoracic Outlet Syndrome
- Conventional Treatments for Thoracic Outlet Syndrome
- Acupuncture: A Holistic Approach to TOS Management
- How Acupuncture Works
- Scientific Evidence for Acupuncture in TOS
- Acupuncture for Thoracic Outlet Syndrome: Mechanisms and Benefits
- 1. Pain Management
- 2. Muscle Relaxation and Decompression
- 3. Improved Circulation
- 4. Nerve Function Restoration
- 5. Stress and Anxiety Reduction
- 6. Holistic Systemic Support
- Key Acupoints for Thoracic Outlet Syndrome
- 1. LI15 (Jianyu) – Large Intestine 15
- 2. LI4 (Hegu) – Large Intestine 4
- 3. GB21 (Jianjing) – Gallbladder 21
- 4. SI11 (Tianzong) – Small Intestine 11
- 5. HT3 (Shaohai) – Heart 3
- 6. PC6 (Neiguan) – Pericardium 6
- 7. ST36 (Zusanli) – Stomach 36
- Acupoint Selection and Treatment Protocol
- Integrating Acupuncture with Conventional TOS Care
- 1. Pre-Treatment Preparation
- 2. Adjunctive Therapy During Conservative Treatment
- 3. Post-Surgical Recovery
- 4. Maintenance and Prevention
- Interdisciplinary Collaboration
- Safety and Considerations
- Lifestyle Tips to Support Acupuncture and TOS Management
- Case Studies and Patient Experiences
- Future Directions and Research
- Conclusion
What Is Thoracic Outlet Syndrome?
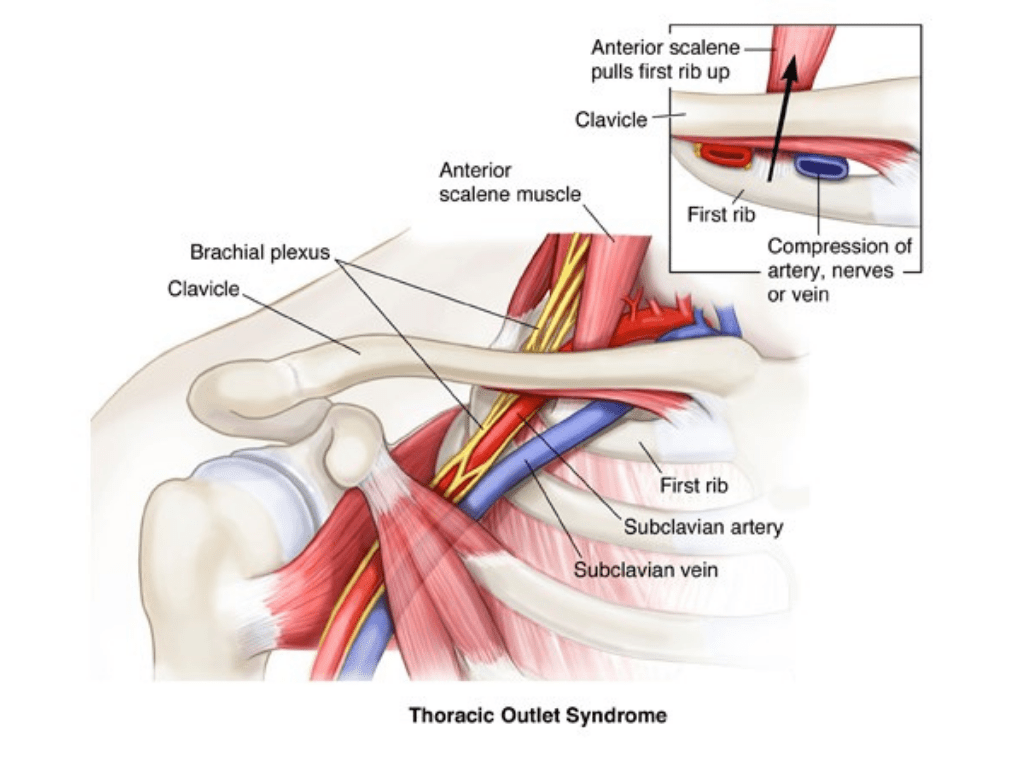
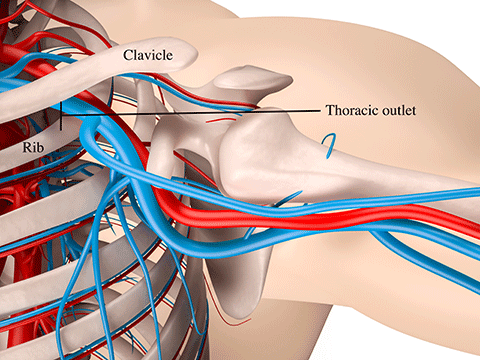
Thoracic Outlet Syndrome refers to a group of disorders caused by the compression of neurovascular structures—specifically, the brachial plexus (nerves), subclavian artery, or subclavian vein—in the thoracic outlet. This anatomical region includes the space between the clavicle (collarbone), the first rib, and the surrounding muscles, such as the scalenes and pectoralis minor. TOS is classified into three main types based on the compressed structure:
Maybe You Need:
- Neurogenic TOS (nTOS): The most common form, accounting for about 95% of cases, involves compression of the brachial plexus, leading to neurological symptoms like pain, numbness, and tingling in the arm, hand, or fingers.
- Vascular TOS (vTOS): Involves compression of the subclavian artery or vein, causing symptoms like swelling, discoloration, or reduced blood flow in the arm.
- Non-Specific or Disputed TOS: A controversial category where symptoms are present but no clear compression is identified, often overlapping with neurogenic TOS.
Prevalence and Risk Factors
TOS affects approximately 1–2% of the general population, with a higher incidence in women and individuals aged 20–50. Risk factors include:
- Anatomical Variations: A cervical rib, elongated transverse process, or tight scalene muscles can narrow the thoracic outlet.
- Poor Posture: Forward head posture, rounded shoulders, or prolonged sitting can compress the thoracic outlet.
- Repetitive Activities: Occupations or activities involving repetitive arm movements (e.g., typing, overhead sports) increase risk.
- Trauma: Whiplash, fractures, or shoulder injuries can trigger TOS.
- Obesity or Muscle Hypertrophy: Excess weight or overdeveloped muscles (e.g., in bodybuilders) can crowd the thoracic outlet.
- Pregnancy: Hormonal changes and posture shifts may contribute to symptoms.
Symptoms of Thoracic Outlet Syndrome
Symptoms vary depending on the type of TOS but commonly include:
- Neurogenic TOS:
- Pain or aching in the neck, shoulder, or arm
- Numbness or tingling in the fingers or hand
- Weakness in the hand or grip
- Muscle wasting in severe cases
- Vascular TOS:
- Swelling or puffiness in the arm or hand
- Bluish discoloration (cyanosis)
- Coldness or temperature changes in the hand
- Pulsating lump above the collarbone
- General Symptoms:
- Fatigue in the arm with activity
- Heaviness or tightness in the affected area
- Symptoms worsened by overhead arm movements or prolonged postures
Conventional Treatments for Thoracic Outlet Syndrome
Conventional treatments aim to relieve compression, reduce symptoms, and restore function. They include:
- Conservative Treatments:
- Physical Therapy: Focuses on posture correction, muscle strengthening, and stretching to open the thoracic outlet.
- Pain Management: Nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, or nerve pain medications (e.g., gabapentin).
- Lifestyle Modifications: Ergonomic adjustments, avoiding repetitive arm movements, and weight management.
- Surgical Treatments (for severe or refractory cases):
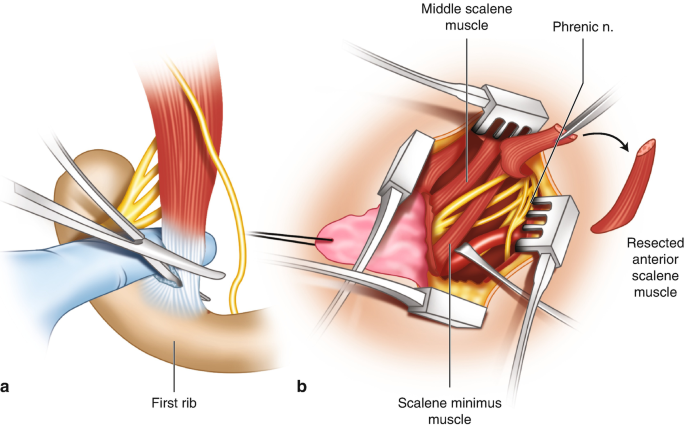
- First Rib Resection: Removal of the first rib or cervical rib to decompress the thoracic outlet.
- Scalenectomy: Removal of part of the scalene muscle to relieve pressure.
- Vascular Repair: Addressing arterial or venous compression in vascular TOS.
While effective for many, these treatments may not fully address chronic pain, stress-related exacerbations, or systemic inflammation, prompting interest in complementary therapies like acupuncture.
Acupuncture: A Holistic Approach to TOS Management
Acupuncture, a key component of Traditional Oriental Medicine (TOM), involves inserting fine, sterile needles into specific points on the body to balance energy flow and promote healing. Used for over 2,500 years, acupuncture is increasingly recognized for its ability to manage pain, reduce inflammation, and improve nerve function, making it a valuable adjunct for TOS.
How Acupuncture Works
In TOM, TOS symptoms are often attributed to blockages in Energy or blood flow along meridians, particularly those affecting the neck, shoulder, and upper limbs. Acupuncture restores balance by stimulating specific points to improve circulation, relax muscles, and reduce inflammation. From a Western perspective, acupuncture’s mechanisms include:
- Pain Relief: Stimulates endorphin release and modulates pain pathways in the central nervous system.
- Anti-Inflammatory Effects: Reduces pro-inflammatory cytokines (e.g., IL-6, TNF-α) and promotes anti-inflammatory mediators.
- Muscle Relaxation: Relieves tension in muscles like the scalenes or pectoralis minor, which contribute to thoracic outlet compression.
- Nerve Regulation: Enhances nerve conduction and reduces neuropathic symptoms like tingling or numbness.
- Stress Reduction: Activates the parasympathetic nervous system, lowering cortisol levels and alleviating stress-related symptom exacerbation.
Scientific Evidence for Acupuncture in TOS
Research on acupuncture for TOS is limited but growing, with studies supporting its efficacy for related conditions like chronic pain, nerve compression, and myofascial syndromes:
- A 2019 study in Pain Medicine found acupuncture reduced pain and improved function in patients with chronic neck and shoulder pain, including those with suspected neurogenic TOS.
- A 2021 review in Complementary Therapies in Clinical Practice reported acupuncture’s effectiveness in reducing neuropathic pain and improving nerve function in peripheral compression syndromes.
- Clinical trials on myofascial pain syndromes, which share similarities with TOS, show acupuncture reduces muscle tension and improves range of motion.
While specific TOS studies are sparse, these findings suggest acupuncture’s potential as a complementary therapy, particularly for neurogenic TOS.

Acupuncture for Thoracic Outlet Syndrome: Mechanisms and Benefits
Acupuncture addresses both the local and systemic aspects of TOS, offering a range of benefits:
1. Pain Management
Chronic pain in the neck, shoulder, or arm is a hallmark of TOS. Acupuncture stimulates the release of endorphins and serotonin, reducing pain perception. It also modulates the brain’s pain processing centers, providing relief without reliance on medications.
2. Muscle Relaxation and Decompression
Tight scalene, pectoralis minor, or trapezius muscles often contribute to thoracic outlet compression. Acupuncture targets trigger points and meridians to relax these muscles, reducing pressure on nerves and blood vessels.
3. Improved Circulation
By enhancing blood flow, acupuncture delivers oxygen and nutrients to compressed tissues, alleviating vascular TOS symptoms like swelling or coldness. It also supports tissue repair in chronic cases.
4. Nerve Function Restoration
Neurogenic TOS involves brachial plexus compression, leading to numbness and weakness. Acupuncture improves nerve conduction and reduces neuropathic symptoms by stimulating peripheral nerves and promoting neural repair.
5. Stress and Anxiety Reduction
Stress exacerbates TOS symptoms by increasing muscle tension and inflammation. Acupuncture’s calming effects, mediated by the parasympathetic nervous system, lower cortisol levels and promote relaxation.
6. Holistic Systemic Support
TOS often coexists with systemic issues like poor posture, stress, or immune dysfunction. Acupuncture addresses these by balancing Energy, supporting immune function, and improving overall vitality.

Key Acupoints for Thoracic Outlet Syndrome
Acupoint selection is tailored to the patient’s TOS type (neurogenic or vascular), symptoms, and TOM diagnosis (e.g., Energy stagnation, blood stasis). Below are key acupoints commonly used for TOS, their locations, and therapeutic effects:
1. LI15 (Jianyu) – Large Intestine 15
- Location: On the shoulder, in the depression anterior and inferior to the acromion when the arm is raised.
- Function: Relieves shoulder pain, improves arm mobility, and relaxes surrounding muscles.
- Application: Effective for shoulder pain and restricted movement in TOS.

2. LI4 (Hegu) – Large Intestine 4
- Location: On the hand, in the webbing between the thumb and index finger.
- Function: A master point for pain relief, particularly in the upper body, and promotes circulation.
- Application: Reduces arm and hand pain, numbness, and tingling in neurogenic TOS.
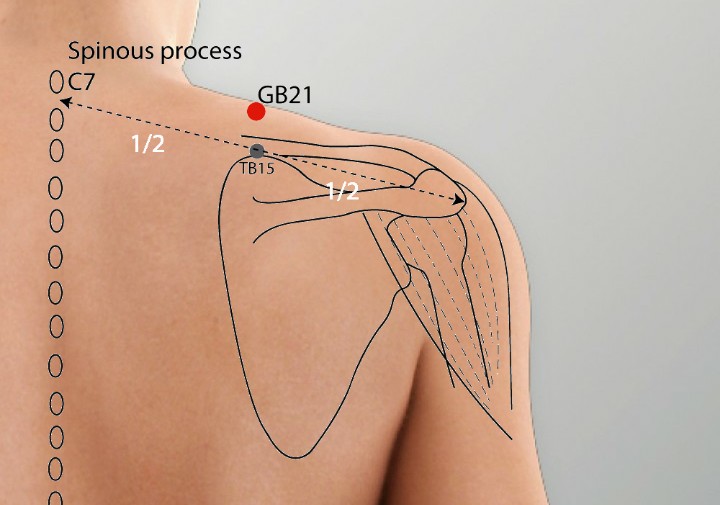
3. GB21 (Jianjing) – Gallbladder 21
- Location: On the shoulder, midway between the base of the neck and the outer tip of the shoulder.
- Function: Relieves neck and shoulder tension, reduces pain, and improves circulation.
- Application: Targets scalene and trapezius muscle tension contributing to TOS compression.
4. SI11 (Tianzong) – Small Intestine 11
- Location: On the scapula, in the depression at the center of the infraspinous fossa.
- Function: Alleviates shoulder and arm pain, relaxes muscles, and improves nerve function.
- Application: Addresses referred pain and numbness in neurogenic TOS.
5. HT3 (Shaohai) – Heart 3
- Location: At the medial end of the elbow crease when the arm is flexed.
- Function: Reduces arm numbness, tingling, and pain; supports nerve function.
- Application: Effective for neuropathic symptoms in the forearm and hand.

6. PC6 (Neiguan) – Pericardium 6
- Location: On the inner forearm, two finger-widths below the wrist crease, between the tendons.
- Function: Calms the mind, reduces stress, and improves circulation to the upper limbs.
- Application: Alleviates stress-related TOS exacerbations and vascular symptoms.
7. ST36 (Zusanli) – Stomach 36
- Location: Below the knee, four finger-widths below the patella, lateral to the shinbone.
- Function: Boosts overall vitality, supports immune function, and enhances healing.
- Application: Addresses systemic factors like fatigue or poor recovery in chronic TOS.
Acupoint Selection and Treatment Protocol
A licensed acupuncturist customizes treatment based on the patient’s TOS type, symptom severity, and TOM diagnosis. A typical protocol includes:
- Initial Assessment: Evaluating symptoms, posture, and TOM patterns (e.g., Energy stagnation, blood stasis, or dampness).
- Needle Insertion: Sterile needles are inserted into 4–8 acupoints for 20–30 minutes per session. Gentle manual stimulation or electro-acupuncture may be used.
- Adjunctive Techniques:
- Electro-Acupuncture: Enhances muscle relaxation and pain relief at points like LI15 and GB21.
- Moxibustion: Warming points like ST36 boosts circulation and healing.
- Cupping: Applied to the upper back or shoulder to relieve muscle tension and improve blood flow.
- Frequency: Weekly sessions for 8–12 weeks, followed by maintenance sessions every 2–4 weeks for chronic cases.
- Duration: Each session lasts 30–60 minutes, depending on the complexity of symptoms.

Integrating Acupuncture with Conventional TOS Care
Acupuncture is most effective as a complementary therapy, enhancing conventional treatments like physical therapy or surgery. Here’s how it can be integrated at various stages of TOS management:
1. Pre-Treatment Preparation
- Purpose: Reduce pain, anxiety, and muscle tension before physical therapy or diagnostic tests (e.g., nerve conduction studies).
- Protocol: Acupuncture sessions targeting LI4, GB21, and PC6 1–2 days before therapy to relax muscles and improve patient comfort.
- Benefits: Enhances tolerance for stretching or manual therapy, reduces stress during medical evaluations.
2. Adjunctive Therapy During Conservative Treatment
- Purpose: Support physical therapy by reducing pain and improving range of motion.
- Protocol: Weekly acupuncture (LI15, SI11, ST36) alongside physical therapy sessions focusing on posture correction and muscle strengthening.
- Benefits: Accelerates symptom relief, reduces reliance on pain medications, and improves therapy outcomes.
3. Post-Surgical Recovery
- Purpose: Minimize post-surgical pain, swelling, and scar tissue formation after procedures like first rib resection.
- Protocol: Acupuncture targeting HT3, LI4, and SP6 within 48 hours post-surgery, followed by weekly sessions for 4–6 weeks.
- Benefits: Speeds recovery, reduces inflammation, and supports nerve regeneration.
4. Maintenance and Prevention
- Purpose: Prevent symptom recurrence and maintain functional improvements.
- Protocol: Monthly acupuncture sessions (ST36, PC6) combined with ongoing physical therapy and ergonomic adjustments.
- Benefits: Sustains pain relief, reduces muscle tension, and supports long-term nerve health.
Interdisciplinary Collaboration
- Dentist/Physician and Acupuncturist Communication: Share diagnostic findings (e.g., imaging, nerve studies) and treatment goals to align care.
- Coordinated Scheduling: Align acupuncture with physical therapy or surgical timelines for optimal results.
- Patient Education: Inform patients that acupuncture complements, not replaces, conventional care, emphasizing the importance of physical therapy and lifestyle changes.
Safety and Considerations
Acupuncture is safe when performed by a licensed practitioner but requires precautions:
- Use sterile, single-use needles to prevent infection.
- Avoid points like GB21 in pregnant patients, as they may induce labor.
- Inform the acupuncturist of medications (e.g., blood thinners) or conditions (e.g., bleeding disorders).
- Coordinate with physicians to ensure acupuncture aligns with TOS treatment plans.
Lifestyle Tips to Support Acupuncture and TOS Management
To maximize the benefits of acupuncture and conventional treatments, patients should adopt:
- Posture Correction:
- Use ergonomic chairs, adjust workstations, and practice shoulder retraction exercises.
- Avoid carrying heavy bags or repetitive overhead movements.
- Exercise and Stretching:
- Perform physical therapy exercises to strengthen the neck and shoulder muscles.
- Incorporate yoga or Pilates to improve posture and flexibility.
- Stress Management:
- Practice mindfulness, meditation, or deep breathing to complement acupuncture’s stress-relieving effects.
- Ensure 7–8 hours of sleep to support recovery.
- Nutrition:
- Eat anti-inflammatory foods (e.g., omega-3-rich fish, berries, leafy greens).
- Stay hydrated to support tissue health.
- Avoid Triggers:
- Limit repetitive activities like typing or sports that exacerbate symptoms.
- Quit smoking to improve vascular health.
/assets/images/provider/photos/2762550.jpg)
Case Studies and Patient Experiences
- Case 1: A 32-year-old office worker with neurogenic TOS experienced reduced arm numbness and shoulder pain after 10 weekly acupuncture sessions (LI15, SI11, PC6) combined with physical therapy.
- Case 2: A 45-year-old athlete with vascular TOS reported less hand swelling and improved circulation after acupuncture (HT3, ST36) post-surgery, with maintenance sessions preventing recurrence.
Future Directions and Research
Future research should focus on:
- Standardized Protocols: Establishing optimal acupoint combinations and session frequencies for TOS.
- Long-Term Outcomes: Evaluating acupuncture’s role in preventing TOS recurrence.
- Mechanistic Studies: Investigating how acupuncture affects nerve conduction and vascular flow in TOS.
- Interdisciplinary Models: Developing clinics that integrate acupuncture, physical therapy, and medical care.
Conclusion
Thoracic Outlet Syndrome is a challenging condition that benefits from a multidisciplinary approach. Acupuncture, with its ability to reduce pain, relax muscles, and improve circulation, complements conventional treatments like physical therapy and surgery. Key acupoints like LI15, GB21, and ST36 target both local and systemic aspects of TOS, offering holistic relief. By integrating acupuncture with conventional care, patients can achieve better symptom management, faster recovery, and improved quality of life. Consult a licensed acupuncturist and your healthcare provider to explore this integrative approach.
Fuji Wellness:
- Address: 132-0031 Matsushima 1-chome, 21-14, Tokyo, Japan
- Chat with us: Click here
- Email: sunnyphamsensei@gmail.com






