Temporal Arteritis and Acupuncture Treatment in Tokyo
Temporal arteritis, also known as giant cell arteritis (GCA), is a chronic inflammatory condition that primarily affects the medium and large arteries, particularly the temporal arteries located on the sides of the head. This condition is a medical emergency due to its potential to cause severe complications, such as vision loss or stroke, if left untreated. It predominantly affects older adults, with a peak incidence in individuals over 50 years of age, and is more common in women and those of Northern European descent.
The condition is characterized by inflammation of the arterial walls, leading to symptoms such as severe headaches, scalp tenderness, jaw pain, and visual disturbances. Conventional treatment relies heavily on corticosteroids to reduce inflammation, but long-term use can lead to significant side effects, prompting interest in complementary therapies like acupuncture. Acupuncture, a cornerstone of Traditional Oriental Medicine (TOM), involves stimulating specific points on the body to restore balance and promote healing. Emerging evidence suggests acupuncture may help manage symptoms of temporal arteritis, reduce inflammation, and improve quality of life, offering a holistic approach to this challenging condition.
This comprehensive article explores temporal arteritis, its causes, symptoms, and conventional treatments, followed by an in-depth look at how acupuncture can be used as a complementary therapy. It also highlights key acupoints used in treatment, providing a detailed guide for patients and practitioners interested in integrative care for temporal arteritis.
- Understanding Temporal Arteritis
- What Is Temporal Arteritis?
- Causes and Risk Factors
- Symptoms and Complications
- Diagnosis
- Conventional Treatments
- Acupuncture for Temporal Arteritis
- What Is Acupuncture?
- How Acupuncture Addresses Temporal Arteritis
- Evidence Supporting Acupuncture for Temporal Arteritis
- Safety and Considerations
- Key Acupoints for Treating Temporal Arteritis
- 1. Taiyang (EX-HN5)
- 2. Fengchi (GB20)
- 3. Yintang (EX-HN3)
- 4. Hegu (LI4)
- 5. Zusanli (ST36)
- 6. Baihui (DU20)
- 7. Neiguan (PC6)
- 8. Yangbai (GB14)
- TOM Perspective on Acupoint Selection
- Acupuncture Techniques
- Integrating Acupuncture with Conventional Treatments
- Practical Considerations for Patients
- Finding a Qualified Acupuncturist
- Treatment Frequency and Duration
- Future Directions and Research Needs
- Conclusion
Understanding Temporal Arteritis
What Is Temporal Arteritis?
Temporal arteritis is a form of vasculitis, an autoimmune condition where the body’s immune system mistakenly attacks its own blood vessels, causing inflammation. The temporal arteries, which supply blood to the head and brain, are most commonly affected, but other arteries, such as the ophthalmic or vertebral arteries, may also be involved. The inflammation causes the arterial walls to thicken, narrowing the blood vessel lumen and reducing blood flow. This can lead to tissue ischemia, particularly in the optic nerve or brain, resulting in serious complications.
Maybe You Need:
The exact cause of temporal arteritis is unknown, but it is thought to involve a combination of genetic, environmental, and immune factors. The condition is closely linked to polymyalgia rheumatica (PMR), another inflammatory disorder that causes muscle pain and stiffness, with up to 50% of GCA patients also experiencing PMR symptoms.
Causes and Risk Factors
Several factors contribute to the development of temporal arteritis:
- Age: The condition primarily affects individuals over 50, with incidence increasing with age.
- Gender: Women are 2–3 times more likely to develop temporal arteritis than men.
- Genetics: A higher prevalence is observed in individuals of Northern European descent, suggesting a genetic predisposition.
- Immune Dysregulation: An overactive immune response triggers inflammation in the arterial walls.
- Environmental Triggers: Infections or other environmental factors may initiate or exacerbate the condition, though specific triggers remain unclear.
Symptoms and Complications
Temporal arteritis presents with a range of symptoms, which may develop gradually or suddenly:
- Headache: A severe, persistent headache, often localized to the temples, is a hallmark symptom.
- Scalp Tenderness: The scalp may be painful to touch, particularly over the temporal arteries.
- Jaw Claudication: Pain or fatigue in the jaw while chewing, due to reduced blood flow.
- Visual Disturbances: Blurred vision, double vision, or sudden vision loss in one eye (amaurosis fugax) may occur. Permanent blindness is a major risk if untreated.
- Systemic Symptoms: Fatigue, fever, weight loss, and muscle aches, often overlapping with PMR.
- Neurological Symptoms: In rare cases, stroke or transient ischemic attacks (TIAs) due to reduced cerebral blood flow.
Untreated temporal arteritis can lead to serious complications, including:
- Blindness: Optic nerve ischemia can cause irreversible vision loss in 15–20% of untreated cases.
- Stroke: Arterial inflammation may lead to blood clots or reduced cerebral blood flow.
- Aneurysms: Chronic inflammation can weaken arterial walls, increasing the risk of aneurysms.
Diagnosis
Diagnosing temporal arteritis requires a combination of clinical evaluation, laboratory tests, and imaging:
- Clinical Assessment: A detailed history and physical exam to identify symptoms like headache, jaw claudication, and scalp tenderness.
- Blood Tests: Elevated erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) indicate inflammation. The interleukin-6 (IL-6) marker may also be elevated.
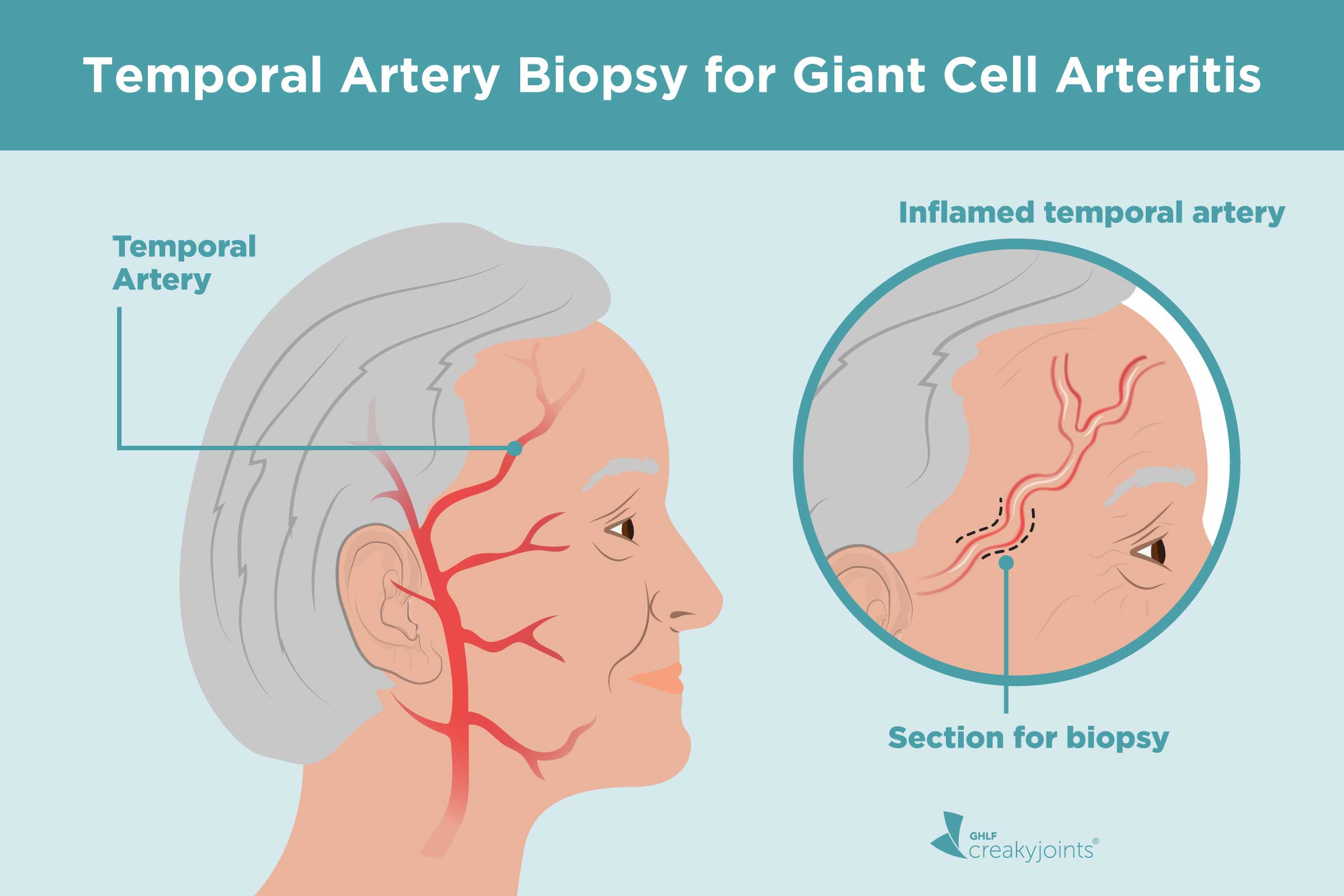
- Temporal Artery Biopsy: A definitive test involving a small sample of the temporal artery to confirm inflammation and giant cell presence.
- Imaging: Ultrasound, MRI, or PET scans can visualize arterial inflammation and guide diagnosis.
Early diagnosis is critical to prevent complications, as delays can lead to irreversible damage.

Conventional Treatments
The primary treatment for temporal arteritis is high-dose corticosteroids, such as prednisone, to rapidly reduce inflammation:
- Corticosteroids: High doses (40–60 mg/day of prednisone) are initiated immediately upon suspicion of GCA, often before biopsy confirmation. Doses are tapered over months or years as symptoms improve.
- Immunosuppressants: Drugs like methotrexate or tocilizumab (an IL-6 inhibitor) may be used to reduce steroid dependence.
- Supportive Therapies: Medications to manage steroid side effects, such as bisphosphonates for bone health or proton pump inhibitors for gastrointestinal protection.
While effective, corticosteroids can cause side effects like osteoporosis, diabetes, weight gain, and increased infection risk, particularly with long-term use. This has led to growing interest in complementary therapies like acupuncture to manage symptoms and reduce reliance on medications.
Acupuncture for Temporal Arteritis
What Is Acupuncture?
Acupuncture is a TOM practice that involves inserting fine, sterile needles into specific acupoints to regulate the flow of energy and blood through meridians, or energy pathways. According to TOM, disease arises from imbalances or blockages in these pathways, and acupuncture restores harmony by stimulating targeted points. Modern science suggests acupuncture may work by modulating the nervous system, releasing anti-inflammatory mediators, and improving blood flow.
For temporal arteritis, acupuncture offers a complementary approach to manage symptoms, reduce inflammation, and improve overall well-being. While not a replacement for corticosteroids, it may help alleviate pain, enhance circulation, and support the body’s natural healing processes.
How Acupuncture Addresses Temporal Arteritis
Acupuncture may benefit temporal arteritis patients through several mechanisms:
- Anti-Inflammatory Effects: Acupuncture has been shown to reduce pro-inflammatory cytokines, such as IL-6 and TNF-α, which are elevated in temporal arteritis. By modulating the immune response, it may help control arterial inflammation.
- Pain Relief: Acupuncture stimulates the release of endorphins and other natural painkillers, alleviating headaches, scalp tenderness, and jaw claudication.
- Improved Blood Flow: By enhancing microcirculation, acupuncture may improve blood supply to affected tissues, reducing ischemic symptoms like vision disturbances.
- Stress Reduction: Chronic stress can exacerbate inflammation. Acupuncture promotes relaxation by activating the parasympathetic nervous system, potentially reducing systemic inflammation.
- Support for Steroid Tapering: Acupuncture may help manage symptoms during corticosteroid dose reduction, minimizing side effects and improving quality of life.

Evidence Supporting Acupuncture for Temporal Arteritis
While research on acupuncture specifically for temporal arteritis is limited, studies on related inflammatory and vascular conditions provide insights:
- Pilot Studies on Vasculitis: Small-scale studies on systemic vasculitis suggest acupuncture reduces inflammation markers (e.g., CRP, ESR) and improves symptoms like pain and fatigue.
- Headache Management: Clinical trials have demonstrated acupuncture’s efficacy for tension-type headaches and migraines, which share features with temporal arteritis-related headaches. A 2016 meta-analysis in The Journal of Pain found acupuncture significantly reduced headache frequency and severity.
- Polymyalgia Rheumatica: Since PMR is closely related to GCA, studies on acupuncture for PMR are relevant. A 2020 study in Acupuncture in Medicine reported improved pain and stiffness in PMR patients receiving acupuncture alongside steroids.
- Anti-Inflammatory Effects: Research in Evidence-Based Complementary and Alternative Medicine (2022) showed acupuncture reduced IL-6 levels in autoimmune conditions, suggesting potential benefits for GCA.
Although direct evidence for temporal arteritis is sparse, these findings support acupuncture’s role as a complementary therapy. Larger, randomized controlled trials are needed to establish its efficacy and optimal protocols.
Safety and Considerations
Acupuncture is generally safe when performed by a licensed practitioner using sterile, single-use needles. Side effects, such as mild bruising or soreness, are rare. For temporal arteritis patients, special considerations include:
- Medical Clearance: Patients on high-dose steroids or with recent vision loss should consult their doctor before starting acupuncture.
- Avoiding Overstimulation: Aggressive needling near inflamed temporal arteries should be avoided to prevent discomfort.
- Monitoring Symptoms: Acupuncture should not delay or replace corticosteroid therapy, especially in acute cases.
Key Acupoints for Treating Temporal Arteritis
Acupoint selection in TOM is based on the patient’s symptoms, meridian imbalances, and underlying pathology. For temporal arteritis, acupoints are chosen to reduce inflammation, improve blood flow, and alleviate pain. Below are key acupoints commonly used, based on TOM principles and clinical experience with inflammatory and vascular conditions:
1. Taiyang (EX-HN5)
- Location: In the depression about one finger-width lateral to the midpoint between the lateral eyebrow and outer canthus of the eye.
- Meridian: Extra Point
- Function: Relieves headaches, reduces inflammation in the head, and improves local blood flow. Taiyang is particularly effective for temporal headaches.
- Clinical Use: Used to alleviate scalp tenderness and temporal artery pain in GCA.

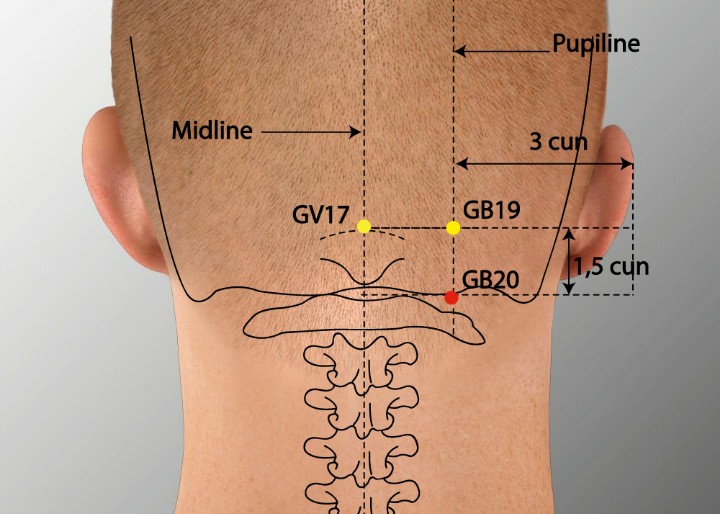
2. Fengchi (GB20)
- Location: At the base of the skull, in the depression between the sternocleidomastoid and trapezius muscles.
- Meridian: Gallbladder
- Function: Promotes blood flow to the head, reduces inflammation, and relieves headache and neck stiffness.
- Clinical Use: GB20 is widely used for headaches and vascular conditions affecting the head, making it ideal for temporal arteritis.
3. Yintang (EX-HN3)
- Location: On the forehead, midway between the eyebrows.
- Meridian: Extra Point
- Function: Calms the mind, reduces stress, and improves cerebral circulation.
- Clinical Use: Helps manage stress-related inflammation and headache in GCA patients.

4. Hegu (LI4)
- Location: On the hand, in the web between the thumb and index finger.
- Meridian: Large Intestine
- Function: Regulates energy and blood, reduces pain, and has systemic anti-inflammatory effects.
- Clinical Use: LI4 is a versatile point for pain relief and immune modulation, supporting symptom management in temporal arteritis.
5. Zusanli (ST36)
- Location: On the anterior aspect of the leg, about four finger-widths below the knee, lateral to the tibia.
- Meridian: Stomach
- Function: Strengthens energy, improves circulation, and reduces systemic inflammation.
- Clinical Use: ST36 is used to boost overall health and reduce inflammatory markers like CRP and IL-6.
6. Baihui (DU20)
- Location: At the top of the head, at the midpoint of the line connecting the apexes of both ears.
- Meridian: Governor Vessel (Du Mai)
- Function: Enhances cerebral blood flow, calms the mind, and regulates energy.
- Clinical Use: DU20 supports brain perfusion and reduces the risk of ischemic complications in GCA.

7. Neiguan (PC6)
- Location: On the inner forearm, approximately two inches above the wrist crease, between the flexor carpi radialis and palmaris longus tendons.
- Meridian: Pericardium
- Function: Regulates cardiovascular function, reduces stress, and improves blood flow.
- Clinical Use: PC6 is used to manage systemic symptoms and support vascular health in GCA.
8. Yangbai (GB14)
- Location: On the forehead, one finger-width above the midpoint of the eyebrow.
- Meridian: Gallbladder
- Function: Relieves frontal headaches and improves local circulation in the head.
- Clinical Use: Effective for addressing forehead pain and visual symptoms associated with temporal arteritis.

TOM Perspective on Acupoint Selection
In TOM, temporal arteritis is often viewed as a condition of “blood stasis” and “heat” in the meridians, particularly those affecting the head (e.g., Gallbladder and Governor Vessel). Acupoints like Taiyang, GB20, and Yintang target local inflammation and pain, while ST36 and PC6 address systemic imbalances. Practitioners may also consider the patient’s TOM diagnosis (e.g., liver yang rising or energy deficiency) to tailor treatment, using pulse and tongue diagnosis to guide acupoint selection.
Acupuncture Techniques
- Manual Acupuncture: Needles are inserted and gently manipulated for 20–30 minutes per session to stimulate energy flow.
- Electroacupuncture (EA): Low-frequency electrical stimulation at points like GB20 and ST36 may enhance anti-inflammatory effects.
- Moxibustion: Applying heat from burning mugwort near acupoints like ST36 can boost energy and circulation, though caution is needed in inflammatory conditions.
- Sham Acupuncture: Used in research as a control, involving superficial needling or non-acupoint stimulation.
Integrating Acupuncture with Conventional Treatments
Acupuncture is most effective as a complementary therapy alongside corticosteroids and other medical treatments:
- With Corticosteroids: Acupuncture may reduce the severity of symptoms, allowing for faster steroid tapering and minimizing side effects.
- With Immunosuppressants: Acupuncture’s immune-modulating effects may enhance the efficacy of drugs like tocilizumab.
- With Lifestyle Changes: Acupuncture supports stress reduction and overall wellness, complementing diet and exercise recommendations.
Patients should work with their healthcare team to integrate acupuncture safely, ensuring it does not interfere with urgent medical interventions.
Practical Considerations for Patients
Finding a Qualified Acupuncturist
- Certification: Choose a practitioner licensed by a recognized body, such as the National Certification Commission for Acupuncture and Oriental Medicine (NCCAOM).
- Experience: Seek acupuncturists with experience in treating inflammatory or vascular conditions.
- Safety: Ensure sterile, single-use needles are used to prevent infections.
Treatment Frequency and Duration
Acupuncture protocols vary, but a typical regimen involves 1–2 sessions per week for 8–12 weeks, with maintenance sessions as needed. Acute cases may require more frequent treatments initially, while chronic management focuses on symptom control.

Future Directions and Research Needs
The use of acupuncture for temporal arteritis is an emerging field, and more research is needed to:
- Conduct randomized controlled trials specifically for GCA to evaluate acupuncture’s efficacy and safety.
- Investigate mechanisms, such as acupuncture’s effects on IL-6 and other inflammatory pathways.
- Develop standardized acupoint protocols for consistent outcomes.
- Assess acupuncture’s role in reducing corticosteroid dependence and improving quality of life.
Ongoing studies, such as those exploring acupuncture for related conditions like PMR, may provide further insights.
Conclusion
Temporal arteritis is a serious inflammatory condition that requires prompt medical intervention to prevent complications like vision loss or stroke. While corticosteroids remain the cornerstone of treatment, acupuncture offers a promising complementary therapy to manage symptoms, reduce inflammation, and improve quality of life. Key acupoints like Taiyang, GB20, ST36, and PC6 target pain, inflammation, and vascular health, aligning with TOM principles of restoring balance.
For patients seeking a holistic approach, acupuncture provides a safe, non-invasive option when performed by a qualified practitioner. It should be integrated with conventional treatments under medical supervision to ensure optimal outcomes. As research continues to explore acupuncture’s benefits, it may become a valuable tool in the management of temporal arteritis, offering hope for improved symptom control and reduced reliance on medications.
If you or a loved one is managing temporal arteritis, consult your healthcare provider to discuss incorporating acupuncture into your treatment plan. Visit our licensed acupuncturist with experience in inflammatory conditions and take a proactive step toward holistic health. Share this article to raise awareness about acupuncture’s potential in addressing this challenging condition.
Fuji Wellness:
- Address: 132-0031 Matsushima 1-chome, 21-14, Tokyo, Japan
- Chat with us: Click here
- Email: sunnyphamsensei@gmail.com




