Post-Traumatic Headache and Acupuncture Treatment in Tokyo
Post-traumatic headache (PTH) is a common and often debilitating condition that develops following a head injury, such as a concussion, traumatic brain injury (TBI), or whiplash. It is one of the most frequent symptoms of post-concussion syndrome, affecting up to 90% of individuals after a head trauma, according to the American Migraine Foundation. PTH can persist for weeks, months, or even years, significantly impacting quality of life, work productivity, and emotional well-being.
Unlike typical headaches, PTH is directly linked to trauma and can present with a variety of symptoms, ranging from mild discomfort to severe, migraine-like pain. Its complex nature often makes it challenging to treat with conventional medications alone, leading many to seek complementary therapies like acupuncture. Rooted in Traditional Oriental Medicine (TOM), acupuncture offers a non-invasive, drug-free approach to managing PTH by reducing pain, calming the nervous system, and promoting overall recovery. This article provides an in-depth exploration of PTH pain, its causes, and how acupuncture can serve as an effective treatment. We’ll also highlight key acupoints used in therapy and offer practical strategies for managing this condition.
- Understanding Post-Traumatic Headache Pain
- Defining Post-Traumatic Headache Pain
- Causes and Risk Factors
- Impact on Daily Life
- Acupuncture Treatment in Tokyo
- How Acupuncture Works for Post-Traumatic Headache
- Scientific Evidence
- Benefits of Acupuncture
- Key Acupoints for Post-Traumatic Headache
- Acupuncture Treatment Protocol
- Integrating Acupuncture with Conventional Treatments
- Lifestyle and Preventive Strategies
- Who Should Consider Acupuncture?
- Choosing a Qualified Acupuncturist
- Potential Challenges and Considerations
- Conclusion
Understanding Post-Traumatic Headache Pain
Defining Post-Traumatic Headache Pain
Post-traumatic headache pain is highly variable, often resembling other headache types such as tension headaches, migraines, or cluster headaches. The International Headache Society classifies PTH as a secondary headache disorder that begins within seven days of a head injury or after regaining consciousness. The pain can be acute (lasting less than three months) or chronic (persisting beyond three months). Common characteristics include:
Maybe You Need:
- Location and Sensation: Pain may be localized to the site of injury or diffuse across the head. It is often described as throbbing, pulsating, pressing, or stabbing.
- Intensity: Ranges from mild to severe, with some patients experiencing debilitating pain that disrupts daily activities.
- Associated Symptoms: Nausea, vomiting, sensitivity to light (photophobia), sound (phonophobia), or smells, dizziness, fatigue, and difficulty concentrating are common, especially in migraine-like PTH.
- Triggers: Pain may worsen with physical exertion, stress, poor sleep, bright lights, loud noises, or certain foods.
- Neck and Shoulder Involvement: Many patients report neck stiffness or shoulder pain, particularly in cases of whiplash-related PTH.
- Intermittent or Constant: Pain may come and go or persist throughout the day, with fluctuations in intensity.
The pain’s complexity arises from its multifactorial origins, including inflammation, nerve irritation, muscle tension, and central nervous system dysregulation following trauma. For some, PTH resolves spontaneously, but for others, it becomes a chronic condition requiring targeted intervention.
Causes and Risk Factors
PTH results from physical, neurological, and biochemical changes triggered by head trauma. Key mechanisms include:
- Inflammation: Trauma causes the release of inflammatory mediators, irritating pain-sensitive structures like the meninges (brain and spinal cord coverings) or cranial nerves.
- Nerve Damage: Injury to the trigeminal nerve or occipital nerves can lead to persistent headache pain.
- Muscle Tension: Trauma to the neck or upper back, as in whiplash, can cause muscle spasms or tightness, contributing to tension-type headaches.
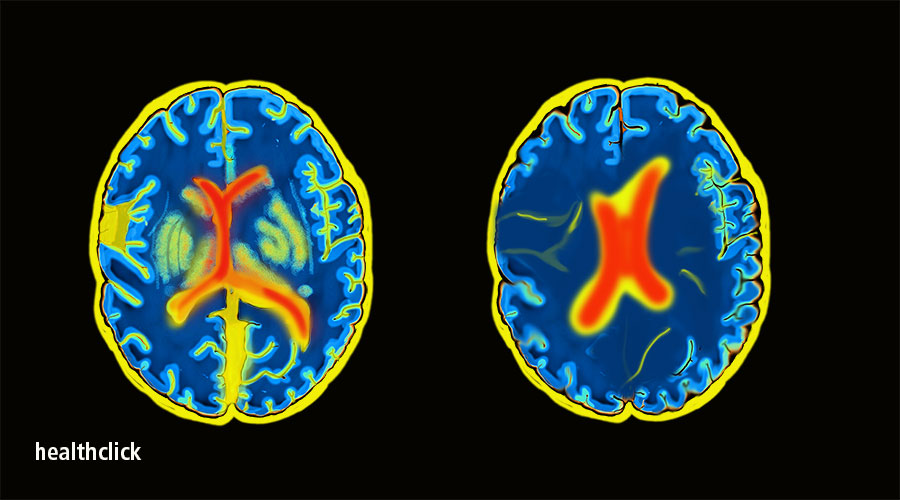
- Central Sensitization: Repeated pain signals can make the brain hypersensitive, amplifying pain perception and lowering the pain threshold.
- Vascular Changes: Altered blood flow or micro-injuries to blood vessels in the brain may trigger migraine-like symptoms.
- Psychological Factors: Stress, anxiety, or post-traumatic stress disorder (PTSD) can exacerbate PTH, creating a feedback loop of pain and emotional distress.
Risk factors include:
- Severity of Injury: More severe TBIs are associated with higher PTH prevalence, though even mild concussions can cause headaches.
- Previous Headaches: A history of migraines or tension headaches increases the likelihood of developing PTH.
- Gender: Women are more likely to develop chronic PTH, possibly due to hormonal or anatomical factors.
- Age: Younger individuals and older adults may be more susceptible to prolonged symptoms.
- Psychosocial Factors: Poor coping mechanisms, depression, or lack of social support can worsen outcomes.
- Repetitive Trauma: Multiple concussions, common in athletes or military personnel, heighten the risk of chronic PTH.

Impact on Daily Life
PTH can profoundly affect daily functioning. Chronic pain may impair concentration, memory, and work performance, leading to reduced productivity or absenteeism. Sleep disturbances, often exacerbated by pain or associated symptoms, contribute to fatigue and irritability. Social activities may be limited due to sensitivity to light, sound, or physical exertion, leading to isolation and emotional distress. The unpredictable nature of PTH can also cause frustration, anxiety, and depression, underscoring the need for effective treatment.
Acupuncture Treatment in Tokyo
Acupuncture, a 2,500-year-old practice from TOM, involves inserting fine, sterile needles into specific acupoints to restore the flow of vital energy and promote healing. For PTH, acupuncture is increasingly recognized as an effective complementary therapy to alleviate pain, reduce inflammation, and calm the nervous system. By addressing both physical and psychological aspects of the condition, acupuncture offers a holistic approach to managing PTH without the side effects of long-term medication use.
How Acupuncture Works for Post-Traumatic Headache
In TOM, PTH is often attributed to blockages in energy and blood flow, typically along the liver meridian, gallbladder meridian, ** or shaoyang meridians, which govern the head and neck. These blockages may result from trauma, blood stasis, or imbalances caused by stress or emotional distress. Acupuncture aims to unblock these pathways, harmonize energy, and reduce pain and inflammation.
From a Western medical perspective, acupuncture’s mechanisms include:
- Pain Modulation: Acupuncture stimulates the release of endorphins, serotonin, and other neurotransmitters that act as natural painkillers, reducing headache intensity.
- Anti-Inflammatory Effects: Needling reduces pro-inflammatory cytokines (e.g., IL-1β, TNF-α), easing inflammation in the meninges, nerves, or soft tissues affected by trauma.
- Nervous System Regulation: Acupuncture modulates the autonomic nervous system, reducing sympathetic overactivity (fight-or-flight response) and promoting parasympathetic activity (rest-and-digest), which helps calm headache triggers.
- Muscle Relaxation: Needling relieves tension and stiffness the neck and shoulder muscles, a common contributor in to tension-type PTH, particularly in whiplash cases.
- Improved Blood Flow: Acupuncture enhances cerebral and local blood flow, reducing vascular irregularities that may trigger migraine-like symptoms.
- Stress Reduction: By regulating cortisol and other stress hormones, acupuncture reduces stress and anxiety, which can amplify pain perception and exacerbate PTH.

Scientific Evidence
Research supports acupuncture’s efficacy for headaches, including PTH. A 2016 meta-analysis in The Journal of Pain found that acupuncture significantly reduced the frequency and intensity of chronic headaches, including those associated with trauma, compared to sham acupuncture or standard care. A 2018 study in Frontiers in Neurology reported that acupuncture reduced headache frequency and improved quality of life in post-concussion patients with chronic PTH, with effects lasting up to six months post-treatment.
Electroacupuncture (EA), which applies a mild electrical current to the needles, has shown particular promise. A 2021 trial in Pain Medicine found that EA was more effective than sham acupuncture in reducing PTH pain intensity and frequency in TBI patients, with 75% of participants reporting significant relief after 8–12 sessions. Another study in Evidence-Based Complementary and Alternative Medicine (2020) highlighted that acupuncture’s ability to modulate neuroinflammation and improve cerebral blood flow, making it a valuable tool for PTH management.
Benefits of Acupuncture
- Non-Invasive: Unlike Unlike invasive procedures like nerve blocks, acupuncture is minimally invasive with few side effects.
- Drug-Free: Avoids side effects of medications like triptans (e.g., rebound headaches) or NSAIDs (e.g., gastrointestinal issues), or opioids (e.g., dependency risks).
- Holistic: Addresses physical pain, neurological symptoms, and emotional stressors like anxiety or PTSD, which often accompany PTH.
- Customizable: Treatments are tailored to the patient’s headache type (e.g., migraine-like vs. tension-type), TOM diagnosis, and overall health.
- Complementary: Can be integrated with conventional treatments like physical therapy, medications, or cognitive behavioral therapy for enhanced outcomes.
Key Acupoints for Post-Traumatic Headache
In TOM, acupoints are selected based on the patient’s symptoms, TOM diagnosis (e.g., liver yang rising, blood stasis), and the affected meridians (primarily liver, gallbladder, and bladder, which govern the head and neck). Practitioners use a combination of local points (on the head and neck) and distal points (on other parts of the body) to address pain, inflammation, and systemic imbalances. Below are the key acupoints commonly used for PTH:
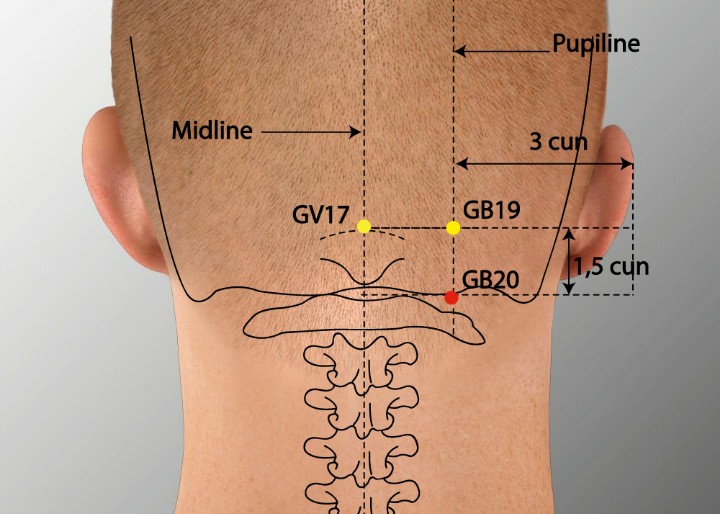
GB20 (Fengchi)
- Location: At the base of the skull, in the depression between the sternocleidomastoid and trapezius muscles, bilaterally.
- Benefits: A primary point for headache relief, GB20 reduces pain in the occipital and temporal regions, relaxes neck muscles, and alleviates dizziness and photophobia. It’s particularly effective for PTH caused by whiplash or neck tension.
- TOM Role: Dispels wind, clears the gallbladder meridian, and promotes Energy flow to the head.
LI4 (Hegu)
- Location: In the webbing between the thumb and index finger on the dorsum of the hand.
- Benefits: A powerful distal point for pain relief throughout the body, LI4 reduces headache severity, stress, and neck tension. It enhances the effects of local head points.
- TOM Role: Regulates the large intestine meridian, promotes Energy circulation, and expels wind.
DU20 (Baihui)
- Location: At the vertex of the head, on the midline, where a line from the apex of the ears intersects.
- Benefits: Calms the mind, reduces headache pain, and improves mental clarity and focus, often impaired in PTH. It’s effective for diffuse or generalized headaches.
- TOM Role: Balances energy in the governing vessel, lifts the spirit, and clears the head.
GB8 (Shuaigu)
- Location: Above the ear, in the temporal region, approximately 1.5 inches above the apex of the auricle.
- Benefits: Relieves migraine-like PTH, reduces temporal pain, and alleviates sensitivity to light and sound.
- TOM Role: Clears the gallbladder meridian, resolves phlegm, and soothes the head.
BL10 (Tianzhu)
- Location: On the back of the neck, just below the occipital bone, lateral to the midline, in the trapezius muscle.
- Benefits: Reduces occipital headache pain, neck stiffness, and dizziness, particularly in whiplash-related PTH.
- TOM Role: Activates the bladder meridian, dispels wind, and promotes circulation to the head.

SP6 (Sanyinjiao)
- Location: On the medial side of the lower leg, three finger-widths above the medial malleolus, posterior to the tibia.
- Benefits: A distal point that reduces stress, promotes relaxation, and supports hormonal balance, which can influence headache triggers. It also improves overall circulation.
- TOM Role: Harmonizes the spleen, liver, and kidney meridians, nourishing yin and calming energy.
LR3 (Taichong)
- Location: On the dorsum of the foot, in the depression between the first and second metatarsal bones.
- Benefits: Relieves headache pain, reduces stress, and regulates emotional imbalances like irritability or anxiety, which can exacerbate PTH.
- TOM Role: Soothes the liver meridian, promotes smooth Energy flow, and resolves stagnation.
SI3 (Houxi)
- Location: On the ulnar side of the hand, in the depression proximal to the fifth metacarpophalangeal joint, when the fist is clenched.
- Benefits: Reduces neck stiffness, occipital pain, and headache, and promotes relaxation. It’s effective for tension-type PTH.
- TOM Role: Activates the small meridian and connects to the governing vessel, clearing head and neck blockages.
Acupuncture Treatment Protocol
Initial Assessment: A licensed acupuncturist evaluates the patient’s medical history, headache characteristics (e.g., location, triggers), and TOM diagnosis (e.g., wind invasion, liver yang rising). Pulse and tongue diagnosis guide point selection.
Session Frequency: Typically 1–2 sessions per week for 6–12 weeks, with maintenance sessions monthly for chronic PTH.
Session Duration: 20–40 minutes, with needles inserted to depths of 0.1–1.5 cm, depending on the point, and retained or gently manipulated.
Adjunct Therapies:
- Electroacupuncture: Mild electrical currents enhance pain relief and reduce neuroinflammation, particularly for severe or chronic PTH.
- Moxibustion: Applying heat from burning mugwort near points like GB20 or DU20 improves circulation and relieves tension.
- Cupping: Suction cups on the neck or upper back reduce muscle tightness and promote relaxation.
- Tui Na: TOM massage may relieve neck and shoulder tension, complementing acupuncture.
Safety: Acupuncture is safe when performed by a licensed practitioner using sterile, single-use needles. Mild side effects like bruising or temporary soreness are rare.

Integrating Acupuncture with Conventional Treatments
Acupuncture is most effective as part of a comprehensive treatment plan. Combining it with other therapies addresses the multifaceted nature of PTH:
- Medications: Short-term use of NSAIDs, triptans, or anticonvulsants may reduce acute headache pain, while acupuncture supports long-term management.
- Physical Therapy: Neck and cranial exercises, posture correction, or manual therapy can relieve muscle tension and improve mobility, particularly in whiplash cases.
- Cognitive Behavioral Therapy (CBT): CBT helps manage stress, anxiety, or PTSD, which can exacerbate PTH.
- Neurorehabilitation: For TBI patients, occupational or vestibular therapy may improve balance, coordination, and cognitive function, complementing acupuncture’s pain relief.
- Lifestyle Modifications: Sleep hygiene, stress management, and trigger avoidance (e.g., caffeine, bright lights) enhance treatment outcomes.
Lifestyle and Preventive Strategies
To maximize acupuncture’s benefits and prevent PTH recurrence, adopt these lifestyle changes:
- Sleep Hygiene: Aim for 7–9 hours of quality sleep in a dark, quiet environment to support neurological recovery and reduce headache triggers.
- Stress Management: Practice mindfulness, meditation, or yoga to lower stress and calm the nervous system. Progressive muscle relaxation can reduce neck tension.
- Hydration and Nutrition: Drink adequate water and consume a balanced diet rich in anti-inflammatory foods (e.g., omega-3s in salmon, antioxidants in berries, magnesium in leafy greens). Avoid known headache triggers like caffeine, alcohol, or processed foods.
- Physical Activity: Engage in low-impact exercises like walking, swimming, or gentle stretching to improve circulation and reduce muscle tension. Avoid high-impact activities that may exacerbate symptoms.
- Posture Correction: Maintain neutral spine alignment during sitting and standing. Use ergonomic chairs or pillows to support the neck.
- Trigger Avoidance: Limit exposure to bright lights, loud noises, or strong odors, and use sunglasses or earplugs as needed.
- Regular Breaks: Take frequent breaks during prolonged sitting or screen time to prevent neck strain and headache onset.
Who Should Consider Acupuncture?
Acupuncture is suitable for most PTH patients, particularly those seeking natural pain relief or experiencing limited response to medications. It’s especially beneficial for:
- Individuals with chronic or recurrent headaches post-trauma.
- Those with medication side effects or contraindications.
- Patients with co-occurring neck pain, stress, or anxiety.
- Individuals preferring non-invasive therapies over injections or surgery.
However, acupuncture may not be appropriate for:
- Individuals with bleeding disorders or those on anticoagulants (due to bruising risk).
- Pregnant women (certain points, like LI4 or SP6, are contraindicated).
- Those with active infections or skin conditions at needling sites.
- Patients with severe needle phobia.
Consult a healthcare provider before starting acupuncture, especially if you have a history of TBI or other neurological conditions.

Choosing a Qualified Acupuncturist
To ensure safe and effective treatment:
- Credentials: Choose a practitioner certified by a recognized body, such as the National Certification Commission for Acupuncture and Oriental Medicine (NCCAOM) in the U.S.
- Experience: Seek acupuncturists with expertise in neurological or headache disorders.
- Hygiene: Verify that the clinic uses sterile, single-use needles and follows infection control protocols.
- Communication: A skilled acupuncturist listens to your symptoms, explains the treatment plan, and adjusts based on your response.
Potential Challenges and Considerations
While acupuncture is generally well-tolerated, patients may encounter:
- Mild Discomfort: Temporary soreness, tingling, or warmth at needling sites, which typically resolves quickly.
- Delayed Results: Pain relief may require 4–8 sessions, especially for chronic PTH.
- Cost: Acupuncture may not be fully covered by insurance, though some plans include it for headache management. Check with your provider.
- Complexity of PTH: Severe TBI-related headaches may require multidisciplinary care, with acupuncture as one component.
Conclusion
Post-traumatic headache is a challenging condition that can persist long after a head injury, causing significant pain and disruption to daily life. Acupuncture offers a promising, evidence-based approach to managing PTH by reducing pain, inflammation, and stress while promoting neurological recovery. Key acupoints like GB20, LI4, and DU20 target headache symptoms and associated neck tension, providing a holistic solution. When integrated with conventional treatments, lifestyle changes, and stress management, acupuncture can significantly improve outcomes for PTH patients.
For those seeking a natural, drug-free option, acupuncture is a valuable tool in the journey toward pain relief and recovery. Consult a licensed acupuncturist to develop a personalized treatment plan tailored to your symptoms and needs. With consistent care and proactive strategies, you can alleviate PTH symptoms and reclaim your quality of life.
Fuji Wellness:
- Address: 132-0031 Matsushima 1-chome, 21-14, Tokyo, Japan
- Chat with us: Click here
- Email: sunnyphamsensei@gmail.com








