Indigestion and Acupuncture Treatment in Tokyo
Indigestion, also known as dyspepsia, is a common digestive issue that affects millions of people worldwide, causing discomfort, pain, and disruption to daily life. Characterized by symptoms like bloating, nausea, and abdominal pain, indigestion can stem from various causes, ranging from dietary habits to stress. While conventional treatments like antacids and dietary changes are standard, many individuals turn to acupuncture, a cornerstone of Traditional Oriental Medicine (TOM), for relief. This comprehensive guide explores indigestion, the nature of its discomfort, how acupuncture can serve as an effective treatment, and the key acupoints used in therapy. By understanding the condition and acupuncture’s role, patients can make informed decisions to manage their symptoms effectively.
- What is Indigestion?
- Causes of Indigestion
- Symptoms of Indigestion
- Understanding the Discomfort of Indigestion
- Types of Discomfort in Indigestion
- Why Discomfort Worsens with Certain Triggers
- Impact on Quality of Life
- What is Acupuncture?
- How Acupuncture Works
- Acupuncture for Indigestion: Benefits and Effectiveness
- Benefits of Acupuncture for Indigestion
- Scientific Evidence Supporting Acupuncture
- Acupuncture vs. Conventional Treatments
- Key Acupoints for Indigestion
- Additional Acupoints
- Acupuncture Treatment Protocol
- Integrating Acupuncture into a Comprehensive Treatment Plan
- 1. Dietary Modifications
- 2. Lifestyle Changes
- 3. Mind-Body Practices
- 4. Conventional Medical Treatments
- Working with Healthcare Providers
- Potential Limitations and Considerations
- Patient Tips for Acupuncture Treatment
- Conclusion
What is Indigestion?
Indigestion is a term used to describe a range of digestive symptoms that occur in the upper abdomen. It is not a disease but a collection of symptoms that can arise from various underlying causes. Indigestion can be occasional or chronic, with symptoms varying in intensity and frequency.
Maybe You Need:
Causes of Indigestion
Indigestion can result from a variety of factors, including:
Dietary Habits:
- Overeating or eating too quickly can overwhelm the stomach’s digestive capacity.
- Consuming fatty, greasy, spicy, or acidic foods can irritate the stomach lining.
- Excessive alcohol, caffeine, or carbonated beverages can disrupt digestion.
Lifestyle Factors:
- Stress and anxiety can impair digestive function by altering gastric motility and acid secretion.
- Lack of physical activity or irregular eating schedules can contribute to symptoms.
Medical Conditions:
- Gastroesophageal Reflux Disease (GERD): Acid reflux can cause indigestion symptoms like heartburn.
- Peptic Ulcers: Sores in the stomach or duodenum can lead to pain and discomfort.
- Gastritis: Inflammation of the stomach lining, often caused by Helicobacter pylori infection or NSAID use.
- Irritable Bowel Syndrome (IBS): Digestive disorders can overlap with indigestion symptoms.
- Gallstones or Pancreatitis: These conditions can disrupt digestion and cause referred pain.
Medications:
- Drugs like NSAIDs, antibiotics, or aspirin can irritate the stomach lining, leading to dyspepsia.
- Certain medications may slow gastric emptying, exacerbating symptoms.
Other Factors:
- Pregnancy can cause indigestion due to hormonal changes and pressure on the stomach.
- Smoking can weaken the digestive system and increase acid production.

Symptoms of Indigestion
Indigestion presents with a range of symptoms, including:
- Abdominal Pain or Discomfort: A burning, aching, or gnawing sensation in the upper abdomen.
- Bloating: A feeling of fullness or tightness in the stomach.
- Nausea: A sensation of needing to vomit, sometimes accompanied by vomiting.
- Belching or Gas: Excessive burping or flatulence due to trapped air.
- Heartburn: A burning sensation in the chest, often confused with GERD.
- Early Satiety: Feeling full after eating a small amount of food.
- Loss of Appetite: Discomfort may reduce the desire to eat.
These symptoms can vary in severity and may occur after meals, during stress, or spontaneously.
Understanding the Discomfort of Indigestion
The discomfort of indigestion is complex, involving physical sensations, digestive dysfunction, and emotional impacts. Understanding its nature is key to appreciating how acupuncture can provide relief.
Types of Discomfort in Indigestion
Abdominal Pain:
- Often described as a burning, gnawing, or cramping sensation in the upper abdomen (epigastric region).
- Pain may be intermittent or constant, worsening after meals or during stress.
- It can range from mild discomfort to severe pain that disrupts daily activities.
Bloating and Fullness:
- Bloating results from gas buildup or slowed gastric emptying, creating a sensation of tightness or distension.
- Early satiety makes patients feel full quickly, limiting food intake.
Nausea and Vomiting:
- Nausea is a common symptom, often triggered by overeating, fatty foods, or stress.
- Vomiting may occur in severe cases, providing temporary relief but indicating a need for medical evaluation.
Heartburn and Belching:
- Heartburn, caused by acid irritation, is often mistaken for GERD but can occur in functional dyspepsia.
- Excessive belching reflects air trapped in the stomach or esophagus.

Why Discomfort Worsens with Certain Triggers
Indigestion symptoms often intensify due to specific triggers:
- Dietary Factors: Fatty or spicy foods slow gastric emptying, increasing bloating and discomfort.
- Stress: Emotional stress disrupts the autonomic nervous system, affecting digestion and acid production.
- Posture and Timing: Lying down after eating or consuming large meals can exacerbate symptoms by impairing digestion.
Impact on Quality of Life
Chronic or recurrent indigestion can significantly affect daily life, leading to:
- Dietary Restrictions: Avoiding trigger foods may limit enjoyment of meals and social dining.
- Sleep Disturbances: Nighttime symptoms like nausea or pain can disrupt sleep, causing fatigue.
- Emotional Strain: Persistent discomfort may lead to anxiety, frustration, or irritability.
- Work and Social Limitations: Symptoms can reduce productivity and make social events challenging.
- Reduced Appetite: Ongoing discomfort may lead to weight loss or nutritional deficiencies.
Given these challenges, finding a treatment that addresses both symptoms and underlying causes is critical. Acupuncture offers a promising, holistic approach to managing indigestion.
What is Acupuncture?
Acupuncture is a therapeutic practice that involves inserting fine, sterile needles into specific points on the body, known as acupoints, to restore balance and promote healing. Rooted in TOM for over 2,000 years, acupuncture is based on the concept of vital energy flowing through meridians. Blockages or imbalances in energy are believed to cause illness, and acupuncture aims to restore harmony.
In modern medicine, acupuncture is recognized for its ability to stimulate the nervous system, regulate bodily functions, and reduce pain. It is widely used for conditions like chronic pain, stress, and digestive disorders, including indigestion.
How Acupuncture Works
Acupuncture’s effects are supported by both TOM principles and scientific mechanisms:
TOM Perspective:
Indigestion is often attributed to imbalances like stomach energy stagnation, spleen deficiency, or liver energy stagnation (stress-related).
Acupuncture harmonizes energy, strengthens digestive function, and clears blockages to alleviate symptoms.
Scientific Perspective:
Nervous System Regulation: Acupuncture stimulates the vagus nerve, improving gastric motility and reducing acid secretion.
Endorphin Release: Needling triggers the release of endorphins and serotonin, reducing pain and promoting relaxation.
Anti-Inflammatory Effects: Acupuncture lowers pro-inflammatory cytokines, reducing stomach irritation.
Gastric Motility: Acupuncture enhances stomach emptying and regulates digestive rhythms, alleviating bloating and nausea.
These mechanisms make acupuncture well-suited for addressing the multifaceted symptoms of indigestion.

Acupuncture for Indigestion: Benefits and Effectiveness
Acupuncture is increasingly recognized as an effective treatment for indigestion, offering a non-invasive, low-risk alternative to medications. Its holistic approach targets both symptoms and underlying causes, making it appealing for patients seeking lasting relief.
Benefits of Acupuncture for Indigestion
Symptom Relief:
- Acupuncture reduces abdominal pain, bloating, nausea, and heartburn by regulating digestive function.
- Patients often experience fewer and less severe symptoms after treatment.
Improved Digestive Health:
- By strengthening the stomach and spleen (in TOM terms), acupuncture enhances digestion and nutrient absorption.
- It addresses related issues like early satiety and loss of appetite.
Reduced Reliance on Medications:
- Acupuncture can decrease the need for antacids, H2 blockers, or proton pump inhibitors (PPIs), which may cause side effects like diarrhea or nutrient deficiencies.
- This is particularly beneficial for patients seeking natural options.
Stress Reduction:
- Stress is a major trigger for indigestion. Acupuncture lowers cortisol levels, promoting relaxation and mitigating stress-related symptoms.
- Improved mental health enhances overall well-being.
Minimal Side Effects:
- When performed by a licensed practitioner, acupuncture is safe, with rare side effects like mild bruising or soreness.
- It avoids the risks of long-term medication use.
Holistic Benefits:
- Acupuncture addresses physical, emotional, and digestive imbalances, improving energy, sleep, and mood.
- It supports overall wellness, which is crucial for chronic indigestion sufferers.
Scientific Evidence Supporting Acupuncture
Research supports acupuncture’s efficacy for indigestion and related digestive disorders:
- A 2019 study in Evidence-Based Complementary and Alternative Medicine found that acupuncture significantly reduced dyspepsia symptoms, including bloating and pain, compared to placebo.
- A 2020 meta-analysis in The American Journal of Oriental Medicine showed that acupuncture improved functional dyspepsia symptoms and quality of life, with effects lasting up to 4 weeks post-treatment.
- A 2021 study in Journal of Gastroenterology and Hepatology demonstrated that acupuncture enhanced gastric motility and reduced epigastric pain in patients with functional dyspepsia.
- Research in Neurogastroenterology and Motility (2022) indicated that acupuncture modulates vagal nerve activity, improving digestive function and symptom control.
While further large-scale studies are needed, existing evidence suggests acupuncture is a valuable therapy for indigestion.

Acupuncture vs. Conventional Treatments
Comparing acupuncture to standard treatments highlights its unique benefits:
- Medications: Antacids, H2 blockers, and PPIs provide quick relief but may cause side effects or dependency. Acupuncture offers a drug-free alternative with fewer risks.
- Dietary Changes: Avoiding trigger foods is effective but may not address underlying imbalances. Acupuncture complements dietary changes by regulating digestion.
- Prokinetics: Drugs that enhance gastric motility can help but carry risks like neurological side effects. Acupuncture naturally improves motility.
- Surgery: Rarely needed for indigestion, surgical options like fundoplication are invasive. Acupuncture is non-invasive and suitable for mild to moderate cases.
Acupuncture can be used alone or alongside conventional treatments, depending on symptom severity.
Key Acupoints for Indigestion
In TOM, acupoints are selected based on the patient’s symptoms, TOM diagnosis (e.g., stomach energy stagnation, spleen deficiency), and overall health. For indigestion, acupoints are chosen to regulate digestion, reduce pain, and relieve stress. Below are key acupoints commonly used, with their locations and effects.
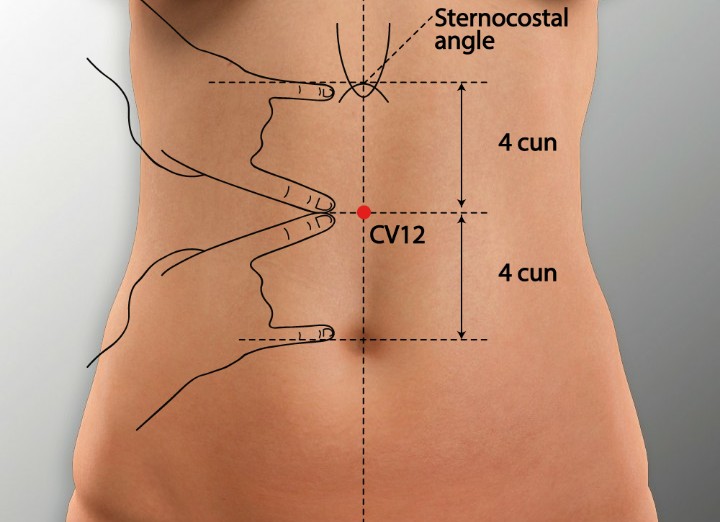
CV12 (Zhongwan) – Middle Cavity
Location: On the midline of the abdomen, 4 cun above the navel.
Function:
Harmonizes the stomach and regulates energy flow.
Relieves epigastric pain, bloating, and nausea.
Enhances gastric motility and digestion.
Application: Ideal for abdominal pain, bloating, and early satiety.
ST36 (Zusanli) – Leg Three Miles
Location: On the outer shin, 3 cun below the knee, one finger’s width from the shinbone.
Function:
Strengthens the stomach and spleen, improving digestion.
Reduces bloating, nausea, and loss of appetite.
Boosts energy and overall digestive health.
Application: Effective for chronic indigestion and weak digestion.
PC6 (Neiguan) – Inner Pass
Location: On the inner forearm, 2 cun above the wrist crease, between the tendons.
Function:
Regulates stomach energy and prevents nausea.
Relieves chest tightness, heartburn, and abdominal discomfort.
Calms the mind, reducing stress-related symptoms.
Application: Used for nausea, vomiting, and stress-induced indigestion.
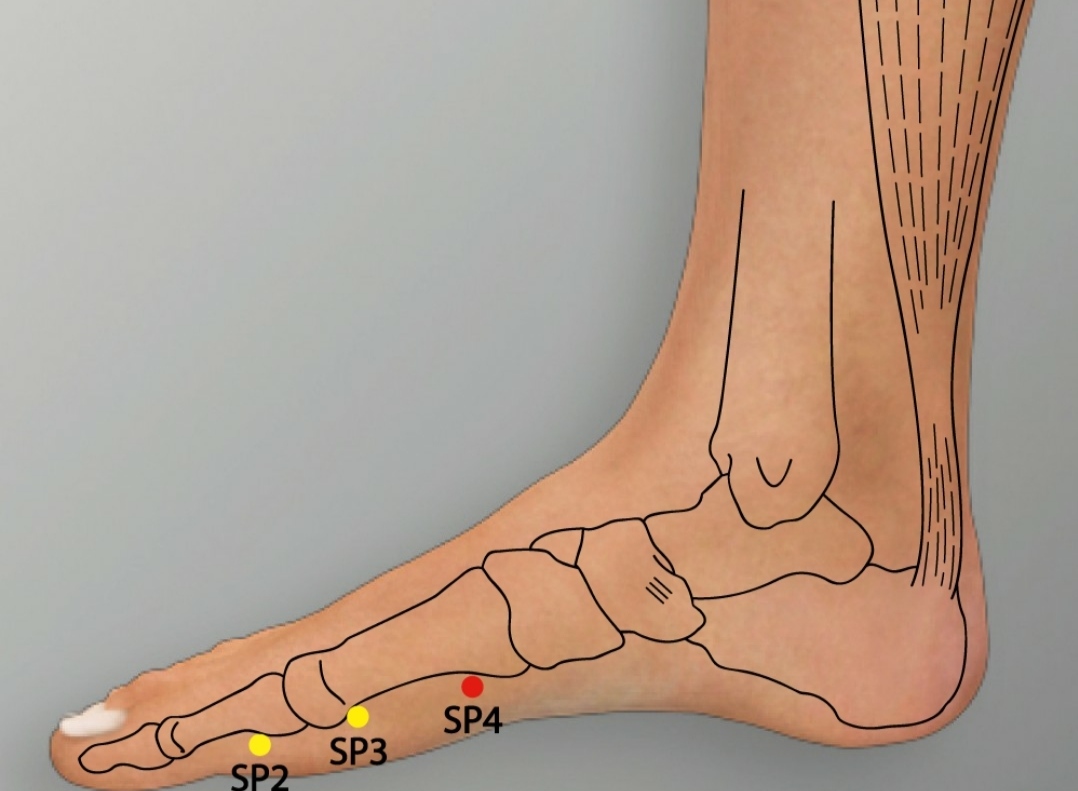
SP4 (Gongsun) – Grandfather Grandson
Location: On the inner foot, in the depression distal to the base of the first metatarsal bone.
Function:
Harmonizes the stomach and spleen, improving digestion.
Alleviates bloating, epigastric pain, and nausea.
Regulates energy flow in the digestive system.
Application: Effective for bloating and sluggish digestion.
LR3 (Taichong) – Great Surge
Location: On the top of the foot, in the depression between the first and second toes.
Function:
Soothes liver energy stagnation, a common cause of stress-related indigestion.
Relieves abdominal tension and emotional stress.
Promotes smooth energy flow.
Application: Used for stress-induced symptoms and epigastric pain.
ST25 (Tianshu) – Celestial Pivot
Location: On the abdomen, 2 cun lateral to the navel.
Function:
Regulates the intestines and stomach, reducing bloating and pain.
Improves bowel function and digestion.
Relieves abdominal distension and discomfort.
Application: Effective for bloating, gas, and irregular digestion.
CV17 (Danzhong) – Chest Center
Location: On the midline of the chest, at the level of the fourth intercostal space.
Function:
Opens the chest, relieving tightness and heartburn.
Regulates energy flow in the upper digestive system.
Calms the mind and reduces stress.
Application: Used for heartburn and stress-related indigestion.

Additional Acupoints
- Local Points: Tender points (ashi points) around the abdomen may be needled to address specific discomfort.
- Distal Points: Points like LI4 (Hegu) on the hand may enhance overall energy flow and pain relief.
Acupuncture Treatment Protocol
A typical acupuncture session for indigestion involves:
- Assessment: The practitioner evaluates symptoms, dietary habits, stress levels, and TOM diagnosis (e.g., spleen deficiency, stomach heat).
- Point Selection: A combination of local (abdomen, chest) and distal (arms, legs) acupoints is chosen based on the patient’s condition.
- Needling: Fine needles are inserted to depths of 0.5–1 inch, depending on the acupoint. Needles remain in place for 20–30 minutes.
- Adjunctive Techniques:
- Electroacupuncture: A mild electrical current enhances stimulation for chronic symptoms.
- Moxibustion: Burning mugwort near acupoints warms the stomach and improves digestion.
- Auricular Acupuncture: Ear points related to the stomach or spleen may be used.
- Frequency: Treatment is typically 1–2 times per week for 6–12 sessions, with adjustments based on response.
Integrating Acupuncture into a Comprehensive Treatment Plan
Acupuncture is most effective when combined with other strategies to manage indigestion holistically.
1. Dietary Modifications
- Avoid Triggers: Limit fatty, spicy, acidic, or gas-producing foods (e.g., beans, carbonated drinks).
- Eat Smaller Meals: Smaller, frequent meals reduce stomach strain and improve digestion.
- Chew Thoroughly: Slow eating aids digestion and prevents air swallowing.
- Complementary Role: Acupuncture enhances digestive efficiency, making dietary changes more effective.
2. Lifestyle Changes
- Stress Management: Practices like meditation, yoga, or deep breathing reduce stress-related symptoms.
- Physical Activity: Gentle exercise like walking promotes gastric motility.
- Posture and Timing: Avoid lying down immediately after meals to prevent symptoms.
- Complementary Role: Acupuncture’s stress-relieving effects support adherence to lifestyle changes.
3. Mind-Body Practices
- Yoga and Tai Chi: These improve digestion and reduce stress, complementing acupuncture.
- Mindfulness: Meditation helps manage emotional triggers of indigestion.
- Complementary Role: Acupuncture enhances relaxation, amplifying mind-body benefits.
4. Conventional Medical Treatments
- Medications: Acupuncture can reduce reliance on antacids, H2 blockers, or PPIs, minimizing side effects.
- Medical Evaluation: Persistent symptoms should be evaluated to rule out serious conditions like ulcers or pylori infection.
- Complementary Role: Acupuncture enhances the effectiveness of medical treatments.

Working with Healthcare Providers
Patients should consult a gastroenterologist or primary care physician to rule out underlying conditions before starting acupuncture. A licensed acupuncturist with experience in digestive disorders should be chosen for safe, effective care. Coordinated care ensures optimal outcomes.
Potential Limitations and Considerations
While acupuncture is generally safe and effective, there are some considerations:
- Individual Variability: Response varies based on symptom severity, underlying causes, and adherence to treatment.
- Temporary Relief: Some patients may need ongoing sessions for sustained benefits.
- Contraindications: Acupuncture should be modified for patients with bleeding disorders, infections at needle sites, or pacemakers (if using electroacupuncture).
- Cost and Accessibility: Insurance coverage for acupuncture varies, and qualified practitioners may not be available in all areas.
Despite these factors, acupuncture remains a low-risk, high-reward option for many indigestion sufferers.
Patient Tips for Acupuncture Treatment
To maximize the benefits of acupuncture for indigestion:
- Choose a Qualified Practitioner: Select a licensed acupuncturist certified by a body like the National Certification Commission for Acupuncture and Oriental Medicine (NCCAOM).
- Share Detailed Information: Discuss symptoms, diet, stress, and medication use to guide treatment.
- Follow Recommendations: Attend sessions as prescribed and report changes in symptoms.
- Combine with Self-Care: Adopt dietary and lifestyle changes to enhance acupuncture’s effects.
- Be Patient: Symptom relief may take several sessions, especially for chronic indigestion.
Conclusion
Indigestion is a disruptive condition that affects digestion, comfort, and quality of life. Acupuncture offers a safe, effective, and holistic approach to managing symptoms by regulating digestive function, reducing pain, and alleviating stress. By targeting key acupoints, it provides relief from bloating, nausea, and abdominal discomfort without the risks of long-term medication use. When integrated into a comprehensive treatment plan, acupuncture can help patients achieve lasting digestive health and improved well-being.
If you’re considering acupuncture for indigestion, consult a licensed practitioner to create a personalized treatment plan. With the right care, you can find relief and take meaningful steps toward better digestive wellness.
Fuji Wellness:
- Address: 132-0031 Matsushima 1-chome, 21-14, Tokyo, Japan
- Chat with us: Click here
- Email: sunnyphamsensei@gmail.com


