Iliotibial Band Syndrome and Acupuncture Treatment
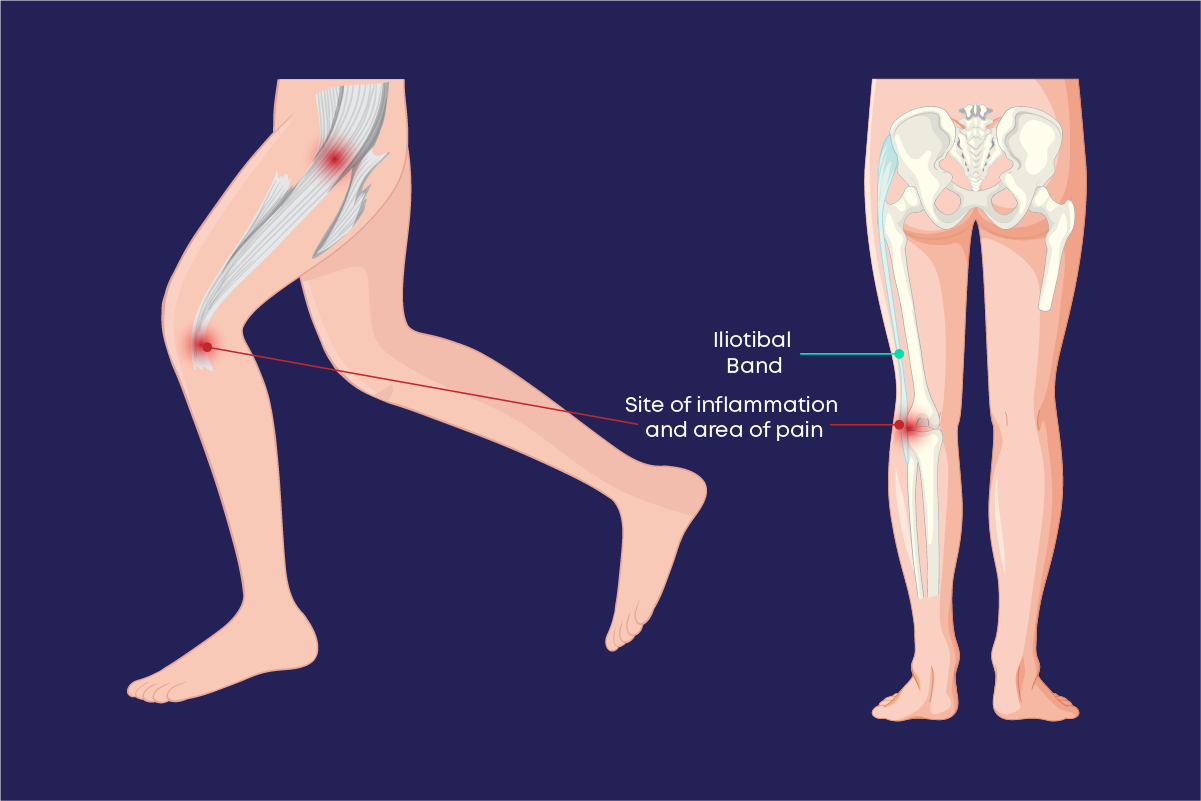
Iliotibial Band Syndrome (ITBS) is a common overuse injury that affects athletes, runners, cyclists, and individuals engaging in repetitive lower-body activities. The iliotibial band (IT band), a thick band of fascia running along the outer thigh from the hip to the knee, plays a crucial role in stabilizing the knee during movement. When the IT band becomes tight, inflamed, or irritated, it can lead to ITBS, characterized by pain on the outer knee or thigh, stiffness, and reduced mobility.
According to the American Academy of Orthopaedic Surgeons (AAOS), ITBS is one of the leading causes of lateral knee pain in runners, with prevalence rates as high as 12% among runners and cyclists. The condition can significantly impact athletic performance and daily activities, making effective treatment essential for recovery and prevention of recurrence. While conventional treatments like rest, physical therapy, and anti-inflammatory medications are widely used, they may not fully address chronic cases or underlying biomechanical issues, prompting many to explore complementary therapies.
Acupuncture, a key practice in traditional Oriental medicine (TOM), has gained attention for its ability to manage musculoskeletal pain and inflammation. By stimulating specific points on the body, acupuncture aims to reduce pain, relax tight tissues, and promote healing, making it a promising option for ITBS. This article provides an in-depth exploration of ITBS, its causes, symptoms, and complications, and examines how acupuncture can complement conventional treatments to support recovery.
- Understanding Iliotibial Band Syndrome: Causes, Symptoms, and Complications
- What Is Iliotibial Band Syndrome?
- Causes of Iliotibial Band Syndrome
- Symptoms of Iliotibial Band Syndrome
- Complications of Iliotibial Band Syndrome
- Conventional Treatments for Iliotibial Band Syndrome
- Acupuncture: A Holistic Approach to Musculoskeletal Pain
- What Is Acupuncture?
- Acupuncture for Iliotibial Band Syndrome: Mechanisms and Applications
- Mechanisms of Acupuncture in ITBS
- Acupoint Selection for ITBS
- TOM Diagnostic Patterns
- Treatment Protocols
- Scientific Evidence
- Benefits of Acupuncture for ITBS
- Risks and Considerations
- Integrating Acupuncture with Conventional Treatment
- Conclusion
Maybe You Need:
Understanding Iliotibial Band Syndrome: Causes, Symptoms, and Complications
What Is Iliotibial Band Syndrome?
Iliotibial Band Syndrome is an overuse injury caused by repetitive friction or compression of the IT band against the lateral femoral epicondyle, a bony prominence just above the knee. The IT band, a dense connective tissue extending from the iliac crest (hip) to the tibia (shin), works with muscles like the tensor fasciae latae (TFL) and gluteus maximus to stabilize the knee and hip during activities like running, cycling, or walking. When the IT band becomes tight or inflamed, it can rub against the femur, leading to pain and dysfunction.
ITBS is often classified as an external (lateral knee pain) or proximal (hip-related) condition, depending on the primary site of symptoms. The condition is most common in individuals who engage in repetitive knee flexion and extension, but it can also affect non-athletes with biomechanical imbalances.
Causes of Iliotibial Band Syndrome
ITBS results from a combination of overuse, biomechanical factors, and training errors. Common causes include:
- Overuse and Repetitive Motion: Activities like running, cycling, or hiking that involve repeated knee bending can strain the IT band, especially without adequate rest.
- Biomechanical Imbalances:
- Weak hip abductors (e.g., gluteus medius) or tight hip flexors, leading to compensatory IT band tension.
- Leg length discrepancies or excessive foot pronation, altering gait mechanics.
- Poor pelvic alignment or core instability, increasing stress on the IT band.
- Training Errors:
- Sudden increases in mileage, intensity, or duration of activity.
- Running on uneven surfaces, downhill slopes, or banked tracks, which stress the lateral knee.
- Inadequate warm-up, stretching, or recovery periods.
- Improper Footwear: Worn-out or unsupportive shoes that fail to correct biomechanical issues.
- Muscle Tightness: Tight quadriceps, hamstrings, or TFL can increase IT band tension, exacerbating irritation.
- Injury or Trauma: Previous injuries to the hip, knee, or lower back may alter movement patterns, contributing to ITBS.
Symptoms of Iliotibial Band Syndrome
ITBS symptoms typically develop gradually and worsen with activity. Common symptoms include:
- Pain Characteristics:
- Sharp, burning, or aching pain on the outer knee, often near the lateral femoral epicondyle.
- Pain that worsens during repetitive activities (e.g., running downhill) and may subside with rest.
- Proximal ITBS may present as pain or tightness in the outer hip or thigh.
- Stiffness and Tightness: Sensation of tightness along the IT band, limiting knee or hip mobility.
- Swelling or Inflammation: Localized swelling or warmth around the lateral knee in severe cases.
- Functional Limitations:
- Difficulty running, climbing stairs, or performing activities requiring knee flexion.
- Pain that starts after a specific distance or duration (e.g., after 2 miles of running).
- Associated Symptoms:
- Clicking or snapping sensations at the knee due to IT band friction.
- Compensatory pain in the hip, lower back, or opposite leg from altered gait.

Complications of Iliotibial Band Syndrome
If untreated, ITBS can lead to complications, including:
- Chronic Pain: Persistent inflammation may cause ongoing pain, even during non-athletic activities.
- Compensatory Injuries: Altered gait or biomechanics can lead to secondary injuries, such as patellofemoral pain syndrome, shin splints, or lower back pain.
- Reduced Athletic Performance: Pain and stiffness may limit training capacity or competitive ability.
- Tissue Scarring: Chronic inflammation can cause adhesions or fibrosis in the IT band, reducing elasticity.
- Psychological Impact: Frustration, anxiety, or depression from prolonged pain and activity restrictions.
Conventional Treatments for Iliotibial Band Syndrome
Conventional treatments focus on reducing inflammation, relieving pain, correcting biomechanics, and preventing recurrence. These include:
- Rest and Activity Modification: Reducing or avoiding aggravating activities (e.g., running) to allow tissue healing.
- Ice and Compression: Applying ice packs and compression wraps to reduce inflammation and swelling.
- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen to manage pain and inflammation.
- Physical Therapy:
- Stretching exercises for the IT band, TFL, and hip flexors.
- Strengthening exercises for the gluteus medius, core, and quadriceps to improve biomechanics.
- Foam rolling or myofascial release to reduce IT band tightness.
- Orthotics or Footwear: Custom orthotics or supportive shoes to correct foot pronation or leg alignment.
- Corticosteroid Injections: For severe cases, injections to reduce localized inflammation.
- Surgical Intervention: Rarely, surgery (e.g., IT band release) is considered for refractory cases.
While these treatments are effective for many, some patients experience persistent symptoms or recurrence, leading them to explore complementary therapies like acupuncture.
Acupuncture: A Holistic Approach to Musculoskeletal Pain
What Is Acupuncture?
Acupuncture, a practice rooted in traditional Oriental medicine for over 2,500 years, involves inserting thin, sterile needles into specific points (acupoints) on the body to promote healing and balance. In TOM, acupuncture restores the flow of vital energy through meridians, correcting imbalances that cause pain or dysfunction.
From a Western perspective, acupuncture works by:
- Stimulating Pain Relief: Needle insertion activates nerve fibers, triggering the release of endorphins, serotonin, and other analgesics.
- Reducing Inflammation: Acupuncture modulates inflammatory cytokines, decreasing swelling and tissue irritation.
- Improving Blood Flow: Stimulation enhances local circulation, promoting tissue repair and reducing muscle tension.
- Relaxing Muscles: Acupuncture can release trigger points and reduce fascial tightness, improving flexibility.

Acupuncture is widely recognized for its efficacy in managing musculoskeletal conditions, including tendonitis, arthritis, and lower back pain. The World Health Organization (WHO) endorses acupuncture for pain relief based on clinical evidence. Given ITBS’s inflammatory and myofascial components, acupuncture’s ability to target these mechanisms makes it a promising therapy.
Acupuncture for Iliotibial Band Syndrome: Mechanisms and Applications
Acupuncture for ITBS is a tailored, holistic approach that aims to alleviate pain, reduce inflammation, release IT band tension, and address biomechanical imbalances. Practitioners customize treatments based on the patient’s symptoms, activity level, and TOM diagnostic patterns, selecting acupoints along the IT band and related meridians. The primary goals of acupuncture for ITBS include:
- Pain Relief: Reducing acute and chronic pain in the lateral knee or hip by modulating pain pathways and releasing natural analgesics.
- Inflammation Reduction: Decreasing localized inflammation to promote healing of the IT band and surrounding tissues.
- Myofascial Release: Relaxing tight muscles (e.g., TFL, gluteus maximus) and fascia to reduce IT band tension.
- Biomechanical Support: Enhancing hip and knee stability by addressing muscle imbalances and improving coordination.
- Stress Reduction: Promoting relaxation to mitigate stress, which can contribute to muscle tightness and pain.
Mechanisms of Acupuncture in ITBS
Acupuncture’s effectiveness for ITBS stems from its multifaceted effects on the musculoskeletal and nervous systems. Key mechanisms include:
- Pain Modulation: Acupuncture stimulates A-delta and C nerve fibers, activating the gate control theory of pain and reducing pain perception. It also upregulates endorphin release, providing natural analgesia for lateral knee or hip pain.
- Anti-Inflammatory Effects: By downregulating pro-inflammatory cytokines (e.g., IL-6, TNF-α) and upregulating anti-inflammatory mediators (e.g., IL-10), acupuncture reduces swelling and irritation at the IT band’s insertion point.
- Myofascial Relaxation: Needle insertion into trigger points or tight fascial bands releases tension in the IT band and associated muscles, improving elasticity and reducing friction against the femur.
- Improved Circulation: Acupuncture enhances local blood flow, delivering oxygen and nutrients to inflamed tissues and aiding repair.
- Neuromuscular Coordination: By stimulating motor points, acupuncture can strengthen weak muscles (e.g., gluteus medius) and improve movement patterns, addressing biomechanical contributors to ITBS.

Acupoint Selection for ITBS
Acupuncturists select points based on the location of pain (knee or hip), TOM patterns, and biomechanical factors. Common acupoints include:
- Local Points:
- GB34 (Yanglingquan): Located below the knee, this point relieves lateral knee pain and relaxes the IT band.
- ST36 (Zusanli): On the shin, it reduces inflammation and supports overall leg health.
- BL40 (Weizhong): At the back of the knee, it alleviates pain and stiffness.
- Distal Points:
- LI4 (Hegu): On the hand, it provides systemic pain relief and reduces muscle tension.
- LV3 (Taichong): On the foot, it regulates qi and reduces stress-related tightness.
- Ashi Points: Tender points along the IT band or TFL are needled to release local tension and pain.
- Hip and Gluteal Points:
- GB30 (Huantiao): Near the hip, it relaxes the gluteus maximus and TFL, reducing proximal ITBS symptoms.
- BL54 (Zhibian): In the gluteal region, it supports hip stability and relieves tension.
- Systemic Points:
- SP6 (Sanyinjiao): On the inner leg, it strengthens qi and supports tissue healing.
- KI3 (Taixi): On the ankle, it nourishes connective tissues and reduces chronic pain.
TOM Diagnostic Patterns
In TOM, ITBS is often associated with patterns like qi stagnation, blood stasis, or damp-cold obstruction. For example:
- Qi Stagnation and Blood Stasis: Sharp, localized pain and tightness, treated with GB34, BL40, and SP10 to invigorate blood and qi.
- Damp-Cold Obstruction: Heavy, aching pain worsened by cold or humidity, treated with SP9 and ST40 to resolve dampness.
- Liver Qi Stagnation: Stress-related tightness and hip pain, treated with LV3 and LI4 to smooth qi flow.
Treatment Protocols
Acupuncture protocols for ITBS depend on the condition’s acuity and severity:
- Acute ITBS: For recent onset, sessions occur 2–3 times per week for 2–4 weeks, focusing on pain relief and inflammation reduction. Electroacupuncture may enhance analgesia by stimulating nerve fibers.
- Chronic ITBS: For persistent symptoms, weekly sessions for 6–12 weeks target pain, myofascial tension, and biomechanical imbalances. Trigger point acupuncture may be used to release adhesions.
- Maintenance Phase: Monthly sessions to prevent recurrence, support flexibility, and maintain muscle balance.
Sessions last 30–60 minutes, with needles retained for 20–30 minutes. Adjunctive therapies like moxibustion (to warm tight muscles), cupping (to release fascia), or Tui Na (to improve circulation) may enhance outcomes.
Scientific Evidence
Research supports acupuncture’s efficacy for musculoskeletal pain, with studies on ITBS showing promise:
- A 2017 study in Journal of Acupuncture and Meridian Studies found acupuncture reduced lateral knee pain in runners with ITBS, improving function after 6 sessions.
- A 2020 meta-analysis in Evidence-Based Complementary and Alternative Medicine confirmed acupuncture’s effectiveness for soft tissue injuries, reducing pain and inflammation.
- A 2019 trial in Pain Medicine reported that electroacupuncture improved outcomes in chronic knee pain, relevant to ITBS.
While more ITBS-specific research is needed, these findings support acupuncture’s role as a complementary therapy.

Benefits of Acupuncture for ITBS
- Non-Invasive: Minimal risk compared to injections or surgery.
- Holistic: Addresses pain, inflammation, and biomechanical factors.
- Customizable: Tailored to the patient’s symptoms and activity level.
- Complementary: Enhances physical therapy and other treatments.
- Preventive: Reduces recurrence by addressing underlying imbalances.
Risks and Considerations
- Qualified Practitioners: Choose a licensed acupuncturist (e.g., NCCAOM-certified).
- Infection Risk: Rare with single-use needles, but sterilization is critical.
- Contraindications: Avoid in patients with severe bleeding disorders or local infections.
- Side Effects: Mild soreness or bruising, typically resolving quickly.
Patients should avoid intense activity immediately after sessions to prevent symptom flare-ups.
Integrating Acupuncture with Conventional Treatment
Acupuncture complements conventional care by:
- Enhancing Pain Relief: Combining with NSAIDs or physical therapy for faster recovery.
- Supporting Rehabilitation: Improving flexibility and strength during physical therapy.
- Preventing Recurrence: Addressing biomechanical issues alongside orthotics or training modifications.
Coordinate with healthcare providers to ensure a cohesive treatment plan.
Lifestyle Tips for ITBS Management:
- Stretching and Foam Rolling: Daily IT band and hip stretches, plus foam rolling to release tension.
- Strengthening: Exercises for gluteus medius and core to improve biomechanics.
- Proper Footwear: Replace shoes every 300–500 miles and consider orthotics.
- Training Modifications: Gradually increase mileage and avoid repetitive downhill running.
- Rest and Recovery: Incorporate rest days and cross-training to reduce overuse.
Conclusion
Iliotibial Band Syndrome is a common yet challenging condition that requires a multifaceted approach. While conventional treatments like rest and physical therapy are effective, acupuncture offers a valuable complementary option for managing pain, reducing inflammation, and improving function. Its holistic nature makes it an appealing choice for athletes and active individuals.
You need acupuncture treatment for Iliotibial Band Syndrome? Contact Fuji Wellness now!
Fuji Wellness:
- Address: 132-0031 Matsushima 1-chome, 21-14, Tokyo, Japan
- Chat with us: Click here
- Email: sunnyphamsensei@gmail.com




