Meningitis Headaches and Acupuncture Treatment in Tokyo
Meningitis is a serious medical condition characterized by inflammation of the meninges, the protective membranes surrounding the brain and spinal cord. One of its hallmark symptoms is severe headaches, which can significantly impact quality of life. While conventional medical treatments are critical for managing meningitis, complementary therapies like acupuncture have gained attention for their potential to alleviate meningitis-related headaches. This article explores meningitis headaches in depth, discusses how acupuncture can serve as a supportive treatment, and highlights key acupoints used in this holistic approach. By combining medical insights with practical information, this guide aims to educate readers and provide actionable steps for those considering acupuncture as a complementary therapy.
- What is Acupuncture?
- Benefits of Acupuncture
- How Acupuncture Treats Meningitis Headaches
- Mechanisms of Action
- Clinical Evidence
- Acupuncture Treatment Protocol for Meningitis Headaches
- Key Acupoints for Meningitis Headaches
- TOM Diagnosis and Customization
- Benefits of Acupuncture for Meningitis Headaches Compared to Conventional Treatments
- Practical Tips for Incorporating Acupuncture into Meningitis Headache Management
- Potential Challenges and Considerations
- FAQs About Meningitis Headaches and Acupuncture
- Conclusion
What is Meningitis?
Maybe You Need:
Meningitis is an inflammation of the meninges, typically caused by infections (viral, bacterial, or fungal) or, less commonly, non-infectious factors such as autoimmune disorders, cancer, or certain medications. The condition can range from mild to life-threatening, with bacterial meningitis requiring urgent medical intervention due to its potential for severe complications, including brain damage or death.

Types of Meningitis
- Bacterial Meningitis:
- Caused by bacteria such as Streptococcus pneumoniae, Neisseria meningitidis, or Haemophilus influenzae.
- Symptoms include severe headaches, high fever, stiff neck, nausea, and sensitivity to light (photophobia).
- Requires immediate treatment with antibiotics and supportive care.
- Viral Meningitis:
- Caused by viruses like enteroviruses, herpes simplex virus, or mumps.
- Generally milder than bacterial meningitis, with symptoms including headaches, fever, and fatigue.
- Often resolves without specific treatment, though supportive care is needed.
- Fungal Meningitis:
- Rare, typically affecting immunocompromised individuals.
- Caused by fungi like Cryptococcus or Histoplasma.
- Symptoms are similar to other forms but may develop more gradually.
- Non-Infectious Meningitis:
- Caused by autoimmune conditions (e.g., lupus), cancers, or drug reactions.
- Headaches and other symptoms vary based on the underlying cause.
Meningitis Headaches: Characteristics and Impact
Meningitis headaches are often described as intense, throbbing, or pressure-like, affecting the entire head or specific areas. Key characteristics include:
- Severity: Often described as one of the worst headaches a person has experienced.
- Associated Symptoms: Stiff neck, fever, photophobia, nausea, vomiting, and confusion.
- Triggers: Movement, light, or sound may worsen the headache.
- Duration: Can persist for days or weeks, depending on the type and treatment of meningitis.
These headaches result from inflammation and increased intracranial pressure caused by the swelling of the meninges. In bacterial meningitis, the rapid progression of symptoms necessitates immediate medical attention, while viral meningitis headaches may resolve with rest and supportive care.
Prevalence and Risk Factors
Meningitis affects people of all ages, but certain groups are at higher risk:
- Infants and Young Children: Due to immature immune systems.
- Adolescents and Young Adults: Particularly for meningococcal meningitis, often spread in close-knit settings like college dorms.
- Immunocompromised Individuals: Those with HIV, cancer, or organ transplants are more susceptible to fungal or opportunistic infections.
- Unvaccinated Populations: Lack of vaccination against H. influenzae, S. pneumoniae, or N. meningitidis increases risk.
Globally, bacterial meningitis causes approximately 250,000 deaths annually, with viral meningitis being more common but less severe. Headaches are a universal symptom across all types, making effective management critical.
Impact on Quality of Life
Meningitis headaches can be debilitating, interfering with daily activities, work, and sleep. In severe cases, they may signal complications like seizures or brain swelling, requiring hospitalization. Even after recovery, some patients experience chronic headaches or neurological issues, highlighting the need for comprehensive treatment strategies.

Conventional Treatments for Meningitis and Associated Headaches
Treating meningitis and its headaches depends on the underlying cause:
- Bacterial Meningitis:
- Intravenous antibiotics (e.g., ceftriaxone, vancomycin) to target the specific bacteria.
- Corticosteroids (e.g., dexamethasone) to reduce inflammation and intracranial pressure.
- Supportive care, including fluids and pain relievers (e.g., acetaminophen, ibuprofen).
- Viral Meningitis:
- Antiviral medications for specific viruses (e.g., acyclovir for herpes-related meningitis).
- Rest, hydration, and over-the-counter pain relievers for symptom relief.
- Fungal Meningitis:
- Antifungal medications (e.g., amphotericin B, fluconazole) for extended periods.
- Management of underlying conditions like HIV.
- Non-Infectious Meningitis:
- Treatment of the underlying cause (e.g., immunosuppressive drugs for autoimmune conditions).
- Pain management with analgesics or anti-inflammatory drugs.
For headaches specifically, nonsteroidal anti-inflammatory drugs (NSAIDs) or opioids may be used, though these carry risks of side effects like gastrointestinal issues or dependency. In cases of persistent post-meningitis headaches, neurologists may recommend preventive medications or physical therapy.
Limitations of Conventional Treatments
While effective for acute meningitis, conventional treatments may not fully address chronic or residual headaches. Side effects of medications, such as nausea or liver toxicity, can also complicate recovery. This has led to growing interest in complementary therapies like acupuncture, which offers a non-invasive approach to headache relief.
What is Acupuncture?
Acupuncture, a cornerstone of Traditional Oriental Medicine (TOM), involves inserting thin, sterile needles into specific points on the body, known as acupoints, to restore balance and promote healing. In TOM, health is maintained by the smooth flow of vital energy through meridians. Blockages or imbalances in Energy are believed to cause illness, and acupuncture aims to correct these disruptions.
From a Western perspective, acupuncture stimulates the nervous system, releases endorphins, and modulates pain signals. These effects make it a promising option for managing headaches, including those associated with meningitis.
Benefits of Acupuncture
Acupuncture is widely used for pain management, stress reduction, and neurological conditions. For meningitis headaches, its potential benefits include:
- Pain Relief: Stimulates endorphin release to reduce headache intensity.
- Anti-Inflammatory Effects: May decrease meningeal inflammation.
- Stress Reduction: Promotes relaxation, addressing stress-related headache triggers.
- Improved Circulation: Enhances blood flow to the brain, potentially relieving pressure-related pain.
When performed by a licensed practitioner, acupuncture is safe with minimal side effects. Potential risks include minor bruising, soreness, or, rarely, infection. Patients with meningitis should only pursue acupuncture after acute infection is resolved and with medical clearance, as active infections require conventional treatment.

How Acupuncture Treats Meningitis Headaches
Acupuncture’s role in managing meningitis headaches lies in its ability to alleviate pain, reduce inflammation, and promote relaxation. Below, we explore the mechanisms, clinical evidence, and practical aspects of using acupuncture for this condition.
Mechanisms of Action
- Pain Modulation: Acupuncture stimulates sensory nerves, activating pain-relieving pathways in the brain and spinal cord. This can reduce the perception of headache pain.
- Anti-Inflammatory Effects: By modulating immune responses and reducing pro-inflammatory cytokines, acupuncture may help alleviate meningeal inflammation, a key contributor to meningitis headaches.
- Regulation of the Autonomic Nervous System: Acupuncture balances sympathetic and parasympathetic activity, reducing stress and tension that exacerbate headaches.
- Improved Cerebral Blood Flow: Enhanced blood circulation to the brain may relieve pressure-related headaches and support recovery from meningitis-related damage.
Clinical Evidence
Research on acupuncture for meningitis headaches specifically is limited, but studies on acupuncture for other headache types provide relevant insights:
- A 2016 meta-analysis in The Journal of Pain found acupuncture effective for reducing the frequency and intensity of tension-type and migraine headaches, suggesting potential benefits for meningitis-related headaches.
- A 2018 study in Evidence-Based Complementary and Alternative Medicine reported that acupuncture reduced inflammation and pain in patients with neurological conditions, supporting its use in post-meningitis recovery.
- Case reports from TOM practitioners indicate that acupuncture, combined with herbal medicine, can alleviate residual headaches after meningitis treatment.
While more research is needed, these findings suggest acupuncture can be a valuable complementary therapy for meningitis headaches, particularly in the recovery phase.
Acupuncture Treatment Protocol for Meningitis Headaches
A typical acupuncture treatment plan for meningitis headaches involves:
- Initial Assessment: The practitioner evaluates the patient’s medical history, headache characteristics, and TOM diagnosis (e.g., Liver Energy stagnation, Blood stasis, or Damp-Heat).
- Session Frequency: Weekly or biweekly sessions for 6–12 weeks, with maintenance treatments as needed.
- Session Duration: 30–60 minutes, with needles retained for 20–30 minutes.
- Complementary Techniques: Moxibustion, scalp acupuncture, or auricular acupuncture may enhance effects.
Patients should only begin acupuncture after acute meningitis is resolved and with approval from their healthcare provider.
Key Acupoints for Meningitis Headaches
In TOM, acupoints are selected based on the patient’s symptoms and underlying imbalances. For meningitis headaches, points are chosen to relieve pain, reduce inflammation, and calm the nervous system. Below are commonly used acupoints, their locations, and therapeutic effects.
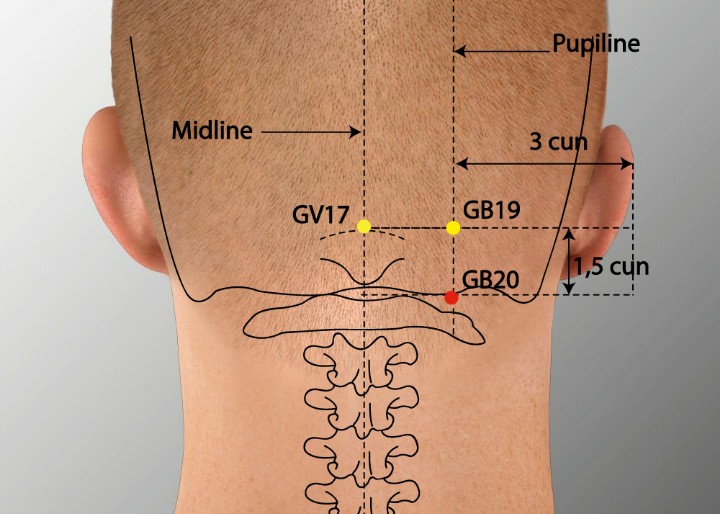
- GB20 (Fengchi) – Gallbladder 20
- Location: At the base of the skull, in the depression between the upper neck muscles.
- Function: Dispels Wind, relieves headache, and clears the head.
- Relevance to Meningitis Headaches: Targets neck stiffness and occipital headaches, common in meningitis.
- LI4 (Hegu) – Large Intestine 4
- Location: On the hand, in the webbing between the thumb and index finger.
- Function: Relieves pain, promotes Energy circulation, and reduces stress.
- Relevance to Meningitis Headaches: Alleviates headache pain and tension, especially in the frontal region.
- Caution: Avoid in pregnant women, as it may induce labor.
- DU20 (Baihui) – Governing Vessel 20
- Location: At the top of the head, in the midline.
- Function: Calms the mind, clears the head, and lifts Energy .
- Relevance to Meningitis Headaches: Addresses generalized headache and mental fog post-meningitis.
- PC6 (Neiguan) – Pericardium 6
- Location: On the inner forearm, about two finger-widths above the wrist crease.
- Function: Calms the mind, regulates Energy , and relieves nausea.
- Relevance to Meningitis Headaches: Reduces stress and nausea, common accompanying symptoms.
- ST36 (Zusanli) – Stomach 36
- Location: On the outer leg, about four finger-widths below the knee and one finger-width lateral to the shinbone.
- Function: Boosts energy, strengthens immunity, and promotes circulation.
- Relevance to Meningitis Headaches: Supports overall recovery and reduces fatigue-related headaches.
- EX-HN3 (Yintang) – Extra Head and Neck 3
- Location: Between the eyebrows, at the midline of the forehead.
- Function: Calms the mind, relieves frontal headaches, and reduces stress.
- Relevance to Meningitis Headaches: Targets frontal pain and promotes relaxation.

Additional Techniques
- Scalp Acupuncture: Points along the scalp corresponding to the sensory cortex may be used to target headache pain.
- Auricular Acupuncture: Ear points for the brain, head, or autonomic nervous system can enhance pain relief.
- Moxibustion: Applying heat to points like ST36 or GB20 can improve circulation and reduce inflammation.
TOM Diagnosis and Customization
In TOM, meningitis headaches may be attributed to patterns like Wind-Heat invasion, Liver Yang rising, or Blood stasis. Acupoints are tailored to the diagnosis:
- Wind-Heat: Focus on GB20 and LI4 to clear heat and relieve pain.
- Liver Yang Rising: Emphasize DU20 and PC6 to calm the mind and reduce tension.
- Blood Stasis: Use ST36 and SP6 (Spleen 6) to promote circulation and resolve stagnation.
A skilled practitioner will adjust the treatment based on pulse, tongue, and symptom analysis.
Benefits of Acupuncture for Meningitis Headaches Compared to Conventional Treatments
Acupuncture offers several advantages for managing meningitis headaches:
- Non-Invasive: Unlike invasive procedures or strong medications, acupuncture has minimal risks.
- Fewer Side Effects: Compared to NSAIDs or opioids, acupuncture rarely causes adverse effects.
- Holistic Approach: Addresses pain, stress, and inflammation simultaneously.
- Customizable: Treatments are tailored to the individual’s symptoms and TOM diagnosis.
- Complementary: Can be safely combined with conventional treatments post-acute phase.
However, acupuncture is not a substitute for medical treatment of active meningitis. It is most effective for residual headaches or as part of a recovery plan.
Practical Tips for Incorporating Acupuncture into Meningitis Headache Management
For those considering acupuncture, here are practical steps:
- Consult Your Doctor:
- Ensure acute meningitis is resolved before starting acupuncture.
- Discuss integration with ongoing treatments.
- Find a Qualified Practitioner:
- Choose a licensed acupuncturist with experience in neurological conditions.
- Verify credentials through organizations like the NCCAOM.
- Communicate Symptoms:
- Share details about headache location, triggers, and associated symptoms.
- Mention any history of meningitis or current medications.
- Commit to Regular Sessions:
- Follow the recommended treatment schedule for best results.
- Support with Lifestyle Changes:
- Stay hydrated and get adequate rest to support recovery.
- Avoid headache triggers like bright lights or loud noises.
- Practice stress management techniques like meditation.
- Monitor Progress:
- Track headache frequency, intensity, and duration.
- Discuss adjustments with your practitioner.
- Check Insurance Coverage:
- Some plans cover acupuncture for chronic pain. Verify with your provider.

Potential Challenges and Considerations
Challenges of using acupuncture for meningitis headaches include:
- Limited Research: Specific studies on acupuncture for meningitis headaches are sparse, though related headache research is promising.
- Cost: Sessions may cost $50–$150, and multiple treatments are often needed.
- Time Commitment: Regular sessions require dedication.
- Variable Response: Some patients experience significant relief, while others see modest benefits.
Patients should weigh these factors and consult their healthcare provider to ensure acupuncture aligns with their treatment plan.
FAQs About Meningitis Headaches and Acupuncture
- Can acupuncture cure meningitis headaches?
Acupuncture cannot cure meningitis but can reduce headache frequency and intensity, especially in the recovery phase.
- Is acupuncture safe during active meningitis?
No, acupuncture should only be used after acute meningitis is resolved and with medical approval.
- How many sessions are needed for relief?
Typically, 6–12 weekly sessions are recommended, followed by maintenance treatments as needed.
- Can acupuncture be combined with medications?
Yes, with medical clearance, acupuncture can complement medications for headache relief.
- Are there risks to acupuncture for meningitis headaches?
Risks are minimal but may include minor bruising or soreness. Serious complications are rare with a licensed practitioner.
Conclusion
Meningitis headaches are a challenging symptom of a serious condition, impacting physical and emotional well-being. While conventional treatments like antibiotics and pain relievers are essential for managing acute meningitis, acupuncture offers a promising complementary approach for alleviating residual headaches. By targeting pain, inflammation, and stress, acupuncture can improve quality of life for those recovering from meningitis. Key acupoints like GB20, LI4, and DU20 address headache-specific symptoms, offering a tailored, holistic treatment.
For those considering acupuncture, working with a qualified practitioner and integrating it with medical care is crucial. With commitment to regular sessions and supportive lifestyle changes, acupuncture can be a valuable tool in managing meningitis headaches. Always consult a healthcare provider to ensure a safe and effective treatment plan.
Fuji Wellness:
- Address: 132-0031 Matsushima 1-chome, 21-14, Tokyo, Japan
- Chat with us: Click here
- Email: sunnyphamsensei@gmail.com




