Ankylosing Spondylitis and Acupuncture Treatment
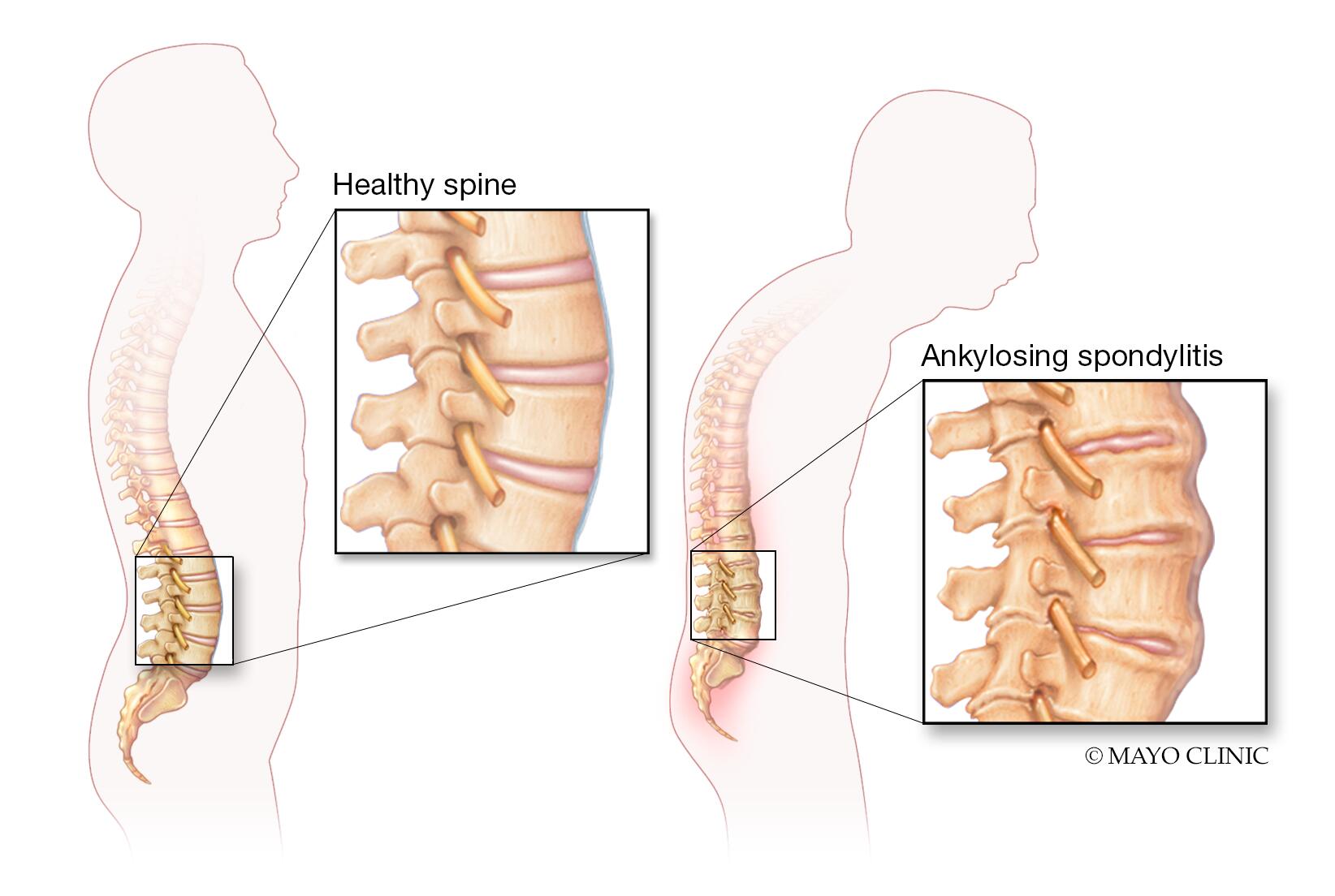
Ankylosing spondylitis (AS) is a chronic inflammatory condition that primarily affects the spine, causing pain, stiffness, and, in severe cases, fusion of the vertebrae. This autoimmune disorder can also impact other joints, such as the hips, shoulders, and knees, and may lead to systemic symptoms like fatigue and inflammation in the eyes (uveitis). While conventional treatments like nonsteroidal anti-inflammatory drugs (NSAIDs), biologics, and physical therapy are standard, many individuals turn to complementary therapies like acupuncture to manage symptoms and improve quality of life.
Acupuncture, a cornerstone of Traditional Oriental Medicine (TOM), involves inserting fine needles into specific points on the body to balance energy flow and promote healing. For ankylosing spondylitis, acupuncture offers a non-invasive, holistic approach to pain relief, reduced inflammation, and improved mobility. This article explores the role of acupuncture in managing AS, with a detailed focus on key acupoints, treatment protocols, and the science behind its efficacy. Whether you’re newly diagnosed or seeking alternative therapies, this guide provides valuable insights into acupuncture as a complementary treatment for AS.
Maybe You Need:
Understanding Ankylosing Spondylitis
Ankylosing spondylitis (AS) is a form of axial spondyloarthritis, a group of inflammatory diseases that affect the spine and other joints. It primarily targets the sacroiliac joints (where the spine connects to the pelvis) and the vertebrae of the spine, causing chronic inflammation that leads to pain and stiffness. Over time, this inflammation can result in the formation of new bone, causing the vertebrae to fuse together, a condition known as ankylosis. This fusion can lead to a loss of spinal flexibility and a characteristic stooped posture.
What Causes Ankylosing Spondylitis?
The exact cause of AS is not fully understood, but it is classified as an autoimmune disorder, meaning the body’s immune system mistakenly attacks its own tissues, leading to inflammation. Key factors associated with AS include:
- Genetic Predisposition: The HLA-B27 gene is strongly linked to AS, present in about 90% of patients with the condition. However, not everyone with the gene develops AS, suggesting other factors play a role.
- Immune System Dysregulation: Abnormal immune responses trigger chronic inflammation in the joints and connective tissues.
- Environmental Triggers: Infections or other environmental factors may activate the disease in genetically susceptible individuals.
- Other Risk Factors: AS is more common in men than women and typically begins in adolescence or early adulthood (before age 45). A family history of AS or related conditions increases the risk.
Symptoms of Ankylosing Spondylitis
AS symptoms vary in severity and may develop gradually. Common signs include:
- Chronic Back Pain and Stiffness: Pain is often felt in the lower back and buttocks, particularly in the sacroiliac joints. It is typically worse in the morning or after periods of inactivity and improves with movement or exercise.
- Neck and Upper Back Pain: As the disease progresses, inflammation may spread to the upper spine, causing stiffness and discomfort.
- Peripheral Joint Involvement: About 30% of AS patients experience pain and swelling in other joints, such as the hips, knees, shoulders, or ankles.
- Fatigue: Chronic inflammation and pain can lead to persistent tiredness, impacting daily energy levels.
- Extra-Articular Symptoms: AS can affect other parts of the body, including:
- Uveitis: Inflammation of the eye, causing redness, pain, and light sensitivity.
- Inflammatory Bowel Disease (IBD): Some patients develop Crohn’s disease or ulcerative colitis.
- Heart Issues: Rarely, AS can lead to aortic inflammation or other cardiovascular complications.
- Postural Changes: In advanced cases, spinal fusion may cause a forward tilt of the spine (kyphosis), leading to a stooped posture.
Symptoms can flare up (exacerbations) and subside (remission), making AS unpredictable. Early diagnosis is critical to prevent irreversible damage.
Impact of Ankylosing Spondylitis
AS can profoundly affect physical, emotional, and social well-being. Chronic pain and stiffness may limit daily activities, such as bending, sitting, or exercising. Fatigue and sleep disturbances due to pain can contribute to stress, anxiety, or depression. In severe cases, spinal fusion may lead to disability, affecting work and personal life. The unpredictable nature of AS flares adds to the emotional burden, making holistic management essential.
Conventional Treatments for Ankylosing Spondylitis
Standard treatments aim to reduce pain, control inflammation, and preserve mobility. These include:
- Medications:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Ibuprofen or naproxen to relieve pain and inflammation.
- Biologics: Tumor necrosis factor (TNF) inhibitors (e.g., adalimumab, etanercept) or interleukin-17 (IL-17) inhibitors (e.g., secukinumab) for severe cases.
- Corticosteroids: Used sparingly for acute flares or uveitis.
- Disease-Modifying Antirheumatic Drugs (DMARDs): Such as sulfasalazine for peripheral joint involvement.
- Physical Therapy: Exercises to maintain spinal flexibility, strengthen muscles, and improve posture.
- Lifestyle Changes: Regular exercise (e.g., swimming, yoga), quitting smoking, and maintaining a healthy weight to reduce joint stress.
- Surgery: Rarely, procedures like spinal osteotomy or joint replacement are needed for severe deformity or hip damage.
While these treatments are effective for many, they may cause side effects (e.g., gastrointestinal issues with NSAIDs, increased infection risk with biologics) or be insufficient for some patients, prompting interest in complementary therapies like acupuncture.

Why Consider Acupuncture for Ankylosing Spondylitis?
Acupuncture has been used for centuries to treat chronic pain and inflammatory conditions. For AS, it offers several potential benefits:
- Pain relief: Acupuncture may reduce back and joint pain by stimulating endorphin release.
- Anti-inflammatory effects: It may modulate inflammatory pathways, addressing the root cause of AS symptoms.
- Improved mobility: By relaxing muscles and improving circulation, acupuncture can enhance spinal and joint flexibility.
- Stress reduction: Chronic pain often leads to stress and anxiety, which acupuncture can alleviate.
- Minimal side effects: Unlike medications, acupuncture has a low risk of adverse effects when performed by a qualified practitioner.
Studies, such as those published in Rheumatology International and The Journal of Alternative and Complementary Medicine, suggest acupuncture can reduce pain and improve function in patients with AS, making it a promising adjunct therapy.
How Acupuncture Works for Ankylosing Spondylitis
In TOM, AS is often attributed to blockages in energy and blood flow, often caused by “wind,” “cold,” “dampness,” or “kidney deficiency” invading the body’s meridians. Acupuncture aims to restore balance by stimulating specific acupoints along these meridians, particularly those associated with the spine, joints, and immune system.
From a biomedical perspective, acupuncture may help AS by:
- Modulating pain pathways: Acupuncture stimulates the release of endorphins, serotonin, and other neurotransmitters, reducing pain perception.
- Reducing inflammation: Needling certain points may decrease pro-inflammatory cytokines like TNF-α and IL-6, which are elevated in AS.
- Improving blood flow: Enhanced circulation delivers oxygen and nutrients to inflamed tissues, promoting healing.
- Regulating the nervous system: Acupuncture may calm the sympathetic nervous system, reducing stress and muscle tension.
- Enhancing joint mobility: By relaxing tight muscles and connective tissues, acupuncture can improve range of motion.
Electroacupuncture, where needles are stimulated with mild electrical currents, is particularly effective for AS, as it can target deeper tissues and provide stronger pain relief.

Key Acupoints for Ankylosing Spondylitis
Acupuncture for AS involves selecting acupoints based on the patient’s symptoms, such as the location of pain (e.g., lower back, hips), the degree of stiffness, and TOM diagnosis (e.g., damp-cold or kidney deficiency patterns). Below is a detailed breakdown of the most commonly used acupoints, their locations, and their therapeutic roles.
- Local Acupoints (Near the Affected Area)
Local acupoints are located near the spine, sacroiliac joints, or other affected areas to directly address pain and inflammation.
- BL23 (Shenshu)
- Location: On the lower back, 1.5 cun lateral to the lower border of the spinous process of the second lumbar vertebra (L2).
- Function: Strengthens the kidneys, nourishes Energy, and relieves lower back pain.
- Application in AS: Targets sacroiliac and lumbar pain, a hallmark of AS. It also supports overall energy and spinal health.
- BL25 (Dachangshu)
- Location: On the lower back, 1.5 cun lateral to the lower border of the spinous process of the fourth lumbar vertebra (L4).
- Function: Alleviates lower back pain and stiffness, regulates the intestines, and reduces inflammation.
- Application in AS: Effective for sacroiliitis and lower back stiffness, especially when pain radiates to the buttocks.
- BL40 (Weizhong)
- Location: At the midpoint of the popliteal crease, behind the knee.
- Function: Relieves back pain, relaxes tendons, and improves circulation in the lower body.
- Application in AS: Used for lower back and leg pain, particularly when AS affects the hips or knees.
- GB30 (Huantiao)
- Location: On the buttock, at the junction of the lateral one-third and medial two-thirds of the line connecting the greater trochanter and the sacral hiatus.
- Function: Relieves hip and lower back pain, strengthens joints, and improves mobility.
- Application in AS: Targets hip pain and sacroiliac inflammation, common in AS.
- BL17 (Geshu)
- Location: On the upper back, 1.5 cun lateral to the lower border of the spinous process of the seventh thoracic vertebra (T7).
- Function: Invigorates blood flow, reduces inflammation, and relieves upper back pain.
- Application in AS: Used for upper spinal stiffness and pain, especially in advanced AS cases.

- Distal Acupoints (Away from the Affected Area)
Distal points are used to address systemic imbalances, reduce inflammation, and promote relaxation.
- LI4 (Hegu)
- Location: On the hand, in the webbing between the thumb and index finger.
- Function: A powerful point for pain relief, regulating Energy, and reducing inflammation throughout the body.
- Application in AS: Helps alleviate generalized pain and inflammation, particularly in the spine and joints.
- LV3 (Taichong)
- Location: On the foot, in the depression between the first and second metatarsal bones.
- Function: Soothes the liver, regulates Energy, and relieves stress and muscle tension.
- Application in AS: Reduces stress-related exacerbations of AS and promotes relaxation of tight muscles.
- SP6 (Sanyinjiao)
- Location: On the inner leg, three finger-widths above the medial malleolus, posterior to the tibia.
- Function: Nourishes blood and yin, calms the nervous system, and reduces inflammation.
- Application in AS: Supports overall relaxation and reduces systemic inflammation.
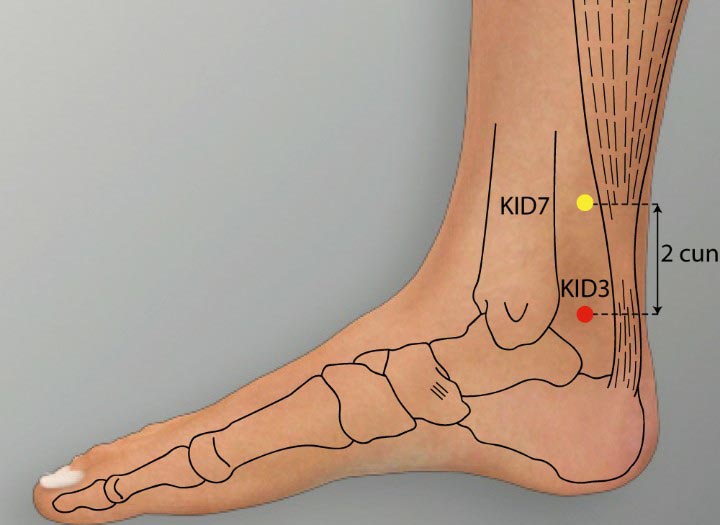
- KI3 (Taixi)
- Location: On the inner ankle, in the depression between the medial malleolus and the Achilles tendon.
- Function: Strengthens the kidneys, nourishes yin, and supports spinal health.
- Application in AS: Addresses fatigue and lower back weakness, common in AS.
- ST36 (Zusanli)
- Location: On the lower leg, four finger-widths below the knee, one finger-width lateral to the tibia.
- Function: Boosts energy, strengthens the immune system, and reduces inflammation.
- Application in AS: Enhances overall vitality and supports immune regulation in autoimmune conditions like AS.
- Extra Points for Ankylosing Spondylitis
Extra points are non-meridian points used for specific conditions like AS.
- Jiaji Points (Huatuojiaji)
- Location: A series of points 0.5–1 cun lateral to the midline of the spine, from T1 to L5.
- Function: Relieves spinal pain and stiffness, improves local circulation, and reduces inflammation.
- Application in AS: Highly effective for addressing pain and stiffness along the entire spine, tailored to the affected vertebrae.
- Yintang
- Location: Between the eyebrows, at the glabella.
- Function: Calms the mind and reduces stress-related pain.
- Application in AS: Helps manage stress and fatigue, which can exacerbate AS symptoms.
- Du14 (Dazhui)
- Location: On the midline of the back, below the spinous process of the seventh cervical vertebra (C7).
- Function: Clears heat, reduces inflammation, and relieves neck and upper back pain.
- Application in AS: Effective for upper spinal stiffness and systemic inflammation.
Acupoint Selection Based on AS Symptoms
The choice of acupoints depends on the patient’s primary symptoms:
- Lower back and sacroiliac pain: BL23, BL25, GB30, BL40, KI3.
- Upper back and neck stiffness: BL17, Du14, Jiaji points, LI4.
- Hip and peripheral joint pain: GB30, SP6, ST36.
- Fatigue and systemic inflammation: KI3, ST36, SP6, LI4.
- Stress and emotional symptoms: LV3, Yintang, PC6.
A skilled acupuncturist may combine local, distal, and extra points, often using 8–12 points per session, to create a personalized treatment plan.
Acupuncture Treatment Protocol for Ankylosing Spondylitis
A typical acupuncture session for AS involves:
- Initial Assessment: The acupuncturist evaluates the patient’s symptoms, medical history, and TOM diagnosis (e.g., damp-cold, kidney deficiency, or blood stagnation).
- Needle Insertion: Sterile, single-use needles are inserted into selected acupoints. The depth and angle vary based on the point’s location and the patient’s condition.
- Stimulation: Manual stimulation (twisting or lifting) or electroacupuncture may be used to enhance effects, particularly for deep spinal or joint pain.
- Session Duration: Needles are typically left in place for 20–30 minutes.
- Frequency: Treatment is often administered 1–2 times per week for 8–12 weeks, with maintenance sessions as needed.
Patients may experience immediate relief or gradual improvement over several sessions. Combining acupuncture with physical therapy, exercise, and dietary changes can enhance outcomes.
Benefits of Acupuncture for Ankylosing Spondylitis
Acupuncture offers several advantages for AS patients:
- Pain Reduction: Studies show acupuncture can reduce pain intensity by up to 40% in chronic inflammatory conditions like AS.
- Improved Mobility: By relaxing muscles and improving joint circulation, acupuncture enhances spinal and peripheral joint flexibility.
- Reduced Inflammation: Acupuncture may lower inflammatory markers, addressing the autoimmune component of AS.
- Enhanced Well-Being: By reducing stress and fatigue, acupuncture improves overall quality of life.
- Complementary Therapy: Acupuncture can be safely combined with medications or physical therapy.
A 2020 study in Clinical Rheumatology found that acupuncture, when combined with conventional treatments, significantly improved pain and function in AS patients compared to standard care alone.
:max_bytes(150000):strip_icc()/Health-GettyImages-1251543001-0beb0933e1ec42ceacfa6b9a9f22335a.jpg)
Safety and Considerations
Acupuncture is generally safe when performed by a licensed practitioner. However, patients should consider:
- Qualified Practitioners: Choose an acupuncturist certified by organizations like the National Certification Commission for Acupuncture and Oriental Medicine (NCCAOM).
- Side Effects: Minor bruising, soreness, or temporary fatigue may occur but are rare.
- Contraindications: Acupuncture may not be suitable for individuals with bleeding disorders, pacemakers (if electroacupuncture is used), or severe skin infections near acupoints.
Always consult a rheumatologist or healthcare provider before starting acupuncture, especially if combining it with biologics or other treatments.
Integrating Acupuncture with Other Therapies
For optimal results, acupuncture can be combined with:
- Medications: NSAIDs or biologics to manage inflammation and pain.
- Physical Therapy: Exercises like stretching or swimming to maintain spinal mobility.
- Dietary Changes: An anti-inflammatory diet rich in omega-3s, fruits, and vegetables to support immune health.
- Lifestyle Modifications: Stress management, adequate sleep, and avoiding prolonged inactivity.
TOM may also recommend herbal remedies or moxibustion to complement acupuncture, particularly for cold-damp patterns.
Finding an Acupuncturist for Ankylosing Spondylitis
To find a qualified acupuncturist:
- Search for licensed practitioners through NCCAOM, the American Association of Acupuncture and Oriental Medicine (AAAOM), or local directories.
- Ask about their experience treating AS or chronic inflammatory conditions.
- Verify that they use sterile, single-use needles and follow safety protocols.
Online platforms like Acupuncture Today or Healthgrades can help locate practitioners specializing in pain and autoimmune disorders.
Conclusion
Acupuncture offers a promising, holistic approach to managing ankylosing spondylitis, providing pain relief, reducing inflammation, and improving mobility. By targeting key acupoints like BL23, GB30, ST36, and Jiaji points, acupuncture addresses both the symptoms and underlying imbalances of AS. When performed by a qualified practitioner, it is a safe, effective complement to conventional treatments. If you’re living with AS, consider consulting a licensed acupuncturist to explore this therapy and develop a personalized treatment plan.
Fuji Wellness:
- Address: 132-0031 Matsushima 1-chome, 21-14, Tokyo, Japan
- Chat with us: Click here
- Email: sunnyphamsensei@gmail.com
.





