Cluster Headaches and How Acupuncture Can Help
Cluster headaches are among the most severe and debilitating types of headaches, often described as excruciating, one-sided pain that can disrupt daily life. Known as “suicide headaches” due to their intensity, cluster headaches affect a small percentage of the population but have a profound impact on those who experience them. While conventional treatments like medications and oxygen therapy are commonly used, complementary therapies such as acupuncture have gained attention for their potential to provide relief. In this we’ll explore the nature of cluster headaches, their causes and symptoms, conventional treatments, and the role of acupuncture, with a detailed focus on its effectiveness and key acupoints for managing this condition.
- What Are Cluster Headaches?
- Causes and Triggers of Cluster Headaches
- Symptoms of Cluster Headaches
- Diagnosing Cluster Headaches
- Conventional Treatments for Cluster Headaches
- Acupuncture Treatment
- Effectiveness of Acupuncture for Cluster Headaches
- Limitations and Considerations
- Key Acupoints for Cluster Headache Relief
- What to Expect During an Acupuncture Session
- Benefits of Acupuncture for Cluster Headaches
- Risks and Considerations
- Lifestyle Tips to Manage Cluster Headaches
- Conclusion
What Are Cluster Headaches?
Cluster headaches are a type of primary headache disorder characterized by intense, unilateral pain, typically centered around one eye or temple. The pain is often described as burning, stabbing, or drilling and is so severe that it can wake sufferers from sleep or make it impossible to function. Unlike migraines, cluster headaches occur in cyclical patterns or “clusters,” with episodes lasting from 15 minutes to 3 hours, often multiple times a day, for weeks or months. These active periods, called cluster bouts, are followed by remission periods with no symptoms.
Maybe You Need:
Cluster headaches are rare, affecting about 0.1% of the population, and are more common in men than women, typically starting between ages 20 and 50. Their exact cause remains unclear, but they are believed to involve abnormal activity in the hypothalamus, blood vessel dilation, and nerve activation.

Causes and Triggers of Cluster Headaches
The precise cause of cluster headaches is not fully understood, but research points to several contributing factors:
- Neurological Factors
- Hypothalamus Dysfunction: The hypothalamus, a brain region that regulates circadian rhythms, is thought to play a central role. Cluster headaches often occur at predictable times, such as during sleep or specific seasons, suggesting a link to the body’s internal clock.
- Trigeminal Nerve Activation: The trigeminal nerve, which transmits pain signals from the face and head, is activated during attacks, contributing to the severe pain.
- Blood Vessel Dilation: Dilated blood vessels in the brain may press on nearby nerves, amplifying pain.
- Genetic Predisposition
- Cluster headaches may have a genetic component, as they can run in families. However, specific genes have not been conclusively identified.
- Triggers
While cluster headaches are not directly caused by external factors, certain triggers can provoke attacks during a cluster bout:
- Alcohol: Even small amounts can trigger an attack within minutes.
- Tobacco and Nicotine: Smoking or exposure to nicotine may increase attack frequency.
- Strong Odors: Perfumes, paint, or gasoline fumes can precipitate episodes.
- Stress or Relaxation: Attacks often occur during periods of relaxation after stress, such as weekends.
- Sleep Changes: Disruptions in sleep patterns, including naps or irregular sleep, can trigger attacks.
- High Altitudes: Air travel or high-altitude environments may provoke episodes.
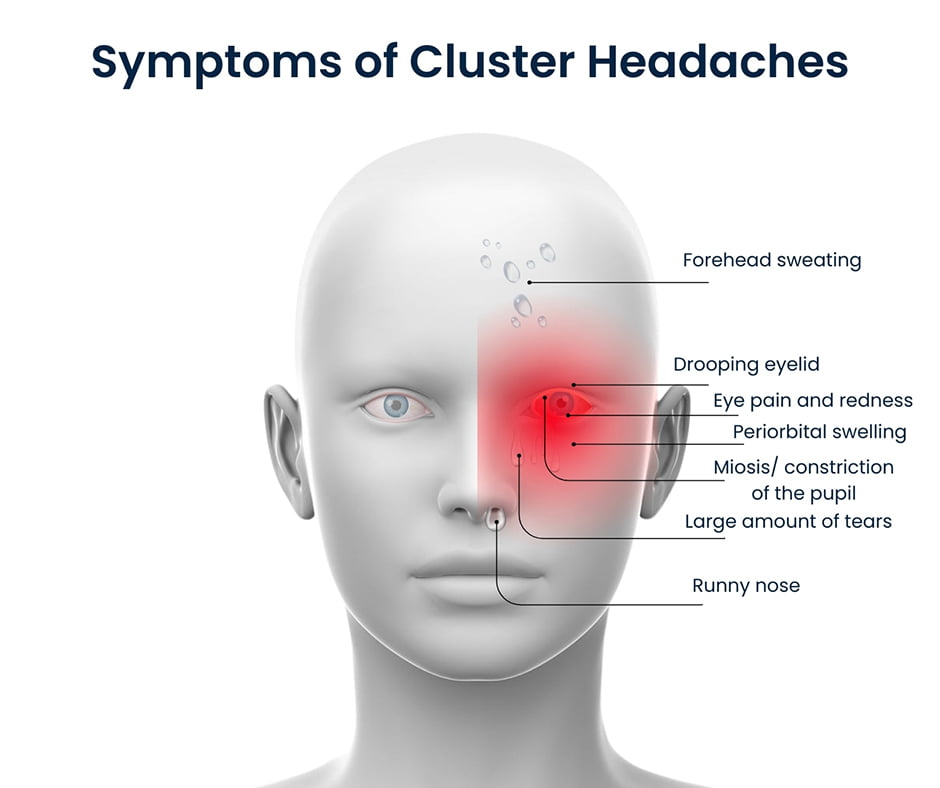
Symptoms of Cluster Headaches
Cluster headaches are unmistakable due to their severity and distinct symptoms, which include:
- Intense, Unilateral Pain: Sharp, burning, or stabbing pain on one side of the head, often around the eye, temple, or forehead.
- Restlessness: Unlike migraine sufferers who seek quiet, cluster headache patients often pace or rock due to the unbearable pain.
- Autonomic Symptoms (on the affected side):
- Drooping eyelid (ptosis)
- Tearing or red eye
- Nasal congestion or runny nose
- Facial sweating or flushing
- Swelling around the eye
- Frequent Attacks: Multiple attacks per day, often at the same time each day or night.
- Short Duration: Attacks last 15 minutes to 3 hours but are intensely painful.
Chronic cluster headaches occur without remission periods or with remissions lasting less than three months, while episodic cluster headaches involve bouts separated by longer remission periods.
Diagnosing Cluster Headaches
Accurate diagnosis is critical to distinguish cluster headaches from other headache disorders like migraines or tension headaches. Diagnosis typically involves:
- Medical History: A detailed account of headache patterns, duration, symptoms, and triggers.
- Physical and Neurological Exam: To rule out other causes, such as brain abnormalities or nerve issues.
- Diagnostic Criteria: Based on the International Classification of Headache Disorders (ICHD-3), cluster headaches are diagnosed if the patient experiences at least five attacks with characteristic symptoms and no other underlying cause.
- Imaging Tests: In rare cases, MRI or CT scans may be ordered to exclude secondary causes like tumors or aneurysms.
Conventional Treatments for Cluster Headaches
Cluster headache treatment focuses on two goals: stopping acute attacks (abortive treatment) and preventing future attacks (preventive treatment).
- Abortive Treatments
- High-Flow Oxygen Therapy: Inhaling 100% oxygen through a mask at 12–15 liters per minute for 15–20 minutes can stop an attack in 70–80% of patients.
- Triptans: Sumatriptan (injected or nasal spray) or zolmitriptan (nasal spray) can relieve pain within minutes but are contraindicated in patients with heart disease.
- Dihydroergotamine (DHE): Administered via injection or nasal spray for severe attacks.
- Lidocaine Nasal Spray: May provide mild relief for some patients.
- Preventive Treatments
- Verapamil: A calcium channel blocker commonly used to reduce attack frequency and severity.
- Corticosteroids: Prednisone or dexamethasone may be prescribed short-term to break a cluster cycle.
- Lithium: Effective for chronic cluster headaches, particularly in patients with mood disorders.
- Nerve Blocks: Occipital nerve blocks with steroids or anesthetics can provide temporary relief.
- Neuromodulation: Devices like sphenopalatine ganglion stimulators or transcranial magnetic stimulation are emerging options for refractory cases.
- Lifestyle Adjustments
- Avoiding known triggers (e.g., alcohol, smoking).
- Maintaining a consistent sleep schedule.
- Managing stress through relaxation techniques.
While effective for many, conventional treatments may cause side effects (e.g., verapamil can cause heart rhythm issues, triptans may cause nausea) or be insufficient for some patients, prompting interest in complementary therapies like acupuncture.

Acupuncture Treatment
Acupuncture is a cornerstone of Traditional Oriental Medicine (TOM) that involves inserting ultra-thin, sterile needles into specific points on the body, known as acupoints. These points are located along meridians, pathways believed to channel the body’s energy. By stimulating acupoints, acupuncture aims to restore energy balance, promote healing, and alleviate pain or discomfort.
Modern research suggests acupuncture works by:
- Triggering the release of endorphins, the body’s natural painkillers.
- Modulating the nervous system to dampen pain signals.
- Improving blood flow and reducing inflammation.
- Regulating autonomic functions, which may help with symptoms like nasal congestion or sweating.
Acupuncture is widely used for pain management, neurological disorders, stress relief, and chronic conditions, making it a promising option for cluster headache sufferers seeking non-pharmacological relief.
Effectiveness of Acupuncture for Cluster Headaches
Acupuncture’s role in treating cluster headaches is an area of growing interest, though research is still emerging. While not a cure, acupuncture may reduce the frequency, intensity, and duration of attacks, improve quality of life, and complement conventional treatments. Below is a detailed exploration of its effectiveness, supported by scientific evidence and clinical observations.
Several studies and reviews have investigated acupuncture’s efficacy for cluster headaches and related headache disorders:
- 2016 Systematic Review (Journal of Headache and Pain): A meta-analysis of acupuncture for primary headaches found moderate evidence that acupuncture reduces headache frequency and intensity compared to sham acupuncture or no treatment. While the review included migraines and tension-type headaches, the mechanisms (e.g., trigeminal nerve modulation) are relevant to cluster headaches.
- 2018 Randomized Controlled Trial (Acupuncture in Medicine): A small study of 30 cluster headache patients showed that acupuncture (10 sessions over 4 weeks) reduced attack frequency by 40% and pain intensity by 30% compared to a control group receiving standard care. Patients also reported improved sleep and reduced reliance on abortive medications.
- 2020 Case Series (Complementary Therapies in Medicine): A report on five chronic cluster headache patients found that acupuncture, combined with verapamil, led to longer remission periods and fewer attacks over 6 months. The authors hypothesized that acupuncture’s effect on the hypothalamus and autonomic nervous system contributed to these outcomes.
- 2021 Study (Pain Research and Management): Research on acupuncture’s neuromodulatory effects showed it can downregulate trigeminal nerve activity and reduce neurogenic inflammation, both key factors in cluster headache pathology.

While these studies are promising, limitations include small sample sizes, variability in acupuncture protocols, and the challenge of blinding in acupuncture trials. Larger, high-quality randomized controlled trials are needed to confirm efficacy specifically for cluster headaches.
Acupuncture may benefit cluster headache sufferers through several mechanisms:
- Pain Modulation: By stimulating acupoints, acupuncture activates the release of endorphins and serotonin, which can reduce the perception of pain. It also influences the descending pain inhibitory pathways in the brain.
- Hypothalamic Regulation: Cluster headaches are linked to hypothalamic dysfunction. Acupuncture may modulate hypothalamic activity, as shown in fMRI studies, potentially stabilizing circadian rhythms and reducing attack triggers.
- Autonomic Balance: Acupuncture can regulate the parasympathetic and sympathetic nervous systems, alleviating autonomic symptoms like tearing, nasal congestion, or eyelid drooping.
- Anti-Inflammatory Effects: By reducing pro-inflammatory cytokines, acupuncture may mitigate neurogenic inflammation in the trigeminal-vascular system.
- Stress Reduction: Stress is a known trigger for cluster headaches. Acupuncture’s calming effect on the nervous system, as evidenced by reduced cortisol levels, may lower attack frequency.
Anecdotal reports from acupuncturists and patients suggest that acupuncture can:
- Shorten the duration of cluster bouts.
- Reduce the need for abortive medications like triptans.
- Improve sleep quality, which is critical for preventing attacks.
- Enhance overall well-being, helping patients cope with the psychological burden of chronic pain.
However, acupuncture’s effectiveness varies between individuals. Factors like the chronicity of the condition, patient response to needling, and the skill of the acupuncturist influence outcomes.
Limitations and Considerations
- Not a Standalone Treatment: Acupuncture is most effective as part of a comprehensive plan, including medications and lifestyle changes.
- Variable Response: Some patients experience significant relief, while others notice minimal improvement.
- Access and Cost: Regular sessions (e.g., 1–2 per week) can be costly ($50–$150 per session), and insurance coverage varies.
- Need for Expertise: Treating cluster headaches requires an acupuncturist skilled in headache management, as precise acupoint selection is critical.
Despite these challenges, acupuncture’s low risk profile and holistic approach make it an appealing option for patients seeking alternatives to medications with side effects.

Key Acupoints for Cluster Headache Relief
Acupuncture for cluster headaches involves stimulating specific acupoints to target pain, autonomic symptoms, and underlying neurological dysfunction. Below are the most commonly used acupoints, their locations, and their therapeutic effects, based on TOM principles and clinical practice:
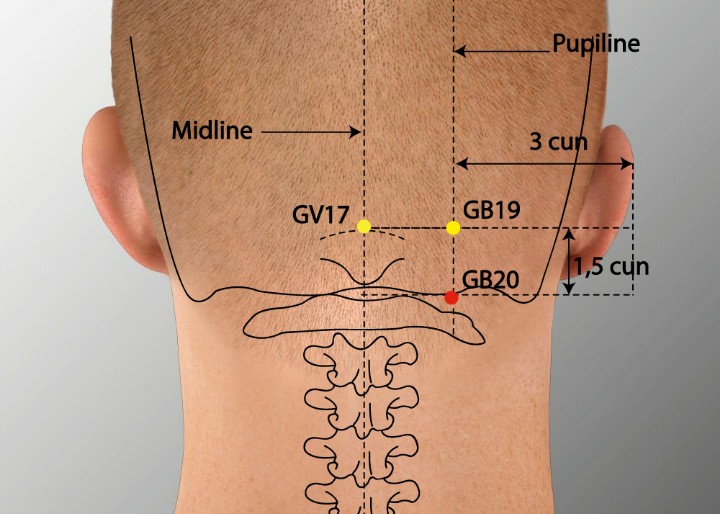
GB20 (Fengchi) – Wind Pool
- Location: At the base of the skull, in the hollows between the upper neck muscles, bilaterally.
- Effects: Relieves headache pain, especially in the occipital and temporal regions. GB20 is a key point for calming the nervous system, reducing stress, and alleviating trigeminal nerve irritation. It also improves blood flow to the head, which may counter vascular dilation.
- Clinical Use: Frequently used in cluster headache protocols due to its proximity to the trigeminal nerve and its ability to address unilateral pain.
LI4 (Hegu) – Joining Valley
- Location: On the hand, in the webbing between the thumb and index finger.
- Effects: A powerful point for pain relief, particularly for head and facial pain. LI4 stimulates endorphin release, reduces inflammation, and promotes relaxation. It’s also used to address autonomic symptoms like nasal congestion.
- Clinical Use: Often combined with other points to enhance overall pain relief and reduce attack intensity.
ST8 (Touwei) – Head Corner
- Location: On the forehead, at the corner of the hairline, about 0.5 inches above the temple.
- Effects: Directly targets frontal and periorbital pain, common in cluster headaches. ST8 also clears “wind” in TOM, which is associated with sharp, sudden pain.
- Clinical Use: Effective for pain around the eye and temple, often needled on the affected side.
EX-HN3 (Yintang) – Hall of Impression
- Location: Between the eyebrows, at the midline of the forehead.
- Effects: Calms the mind, reduces stress, and relieves frontal headache pain. Yintang also regulates the autonomic nervous system, helping with symptoms like tearing or eyelid drooping.
- Clinical Use: Widely used for its soothing effect, especially in patients with stress-triggered attacks.

PC6 (Neiguan) – Inner Gate
- Location: On the inner forearm, about two inches above the wrist crease, between the tendons.
- Effects: Regulates the autonomic nervous system, reduces nausea (sometimes reported in cluster headaches), and promotes relaxation. PC6 also modulates hypothalamic activity, potentially stabilizing circadian rhythms.
- Clinical Use: Included in protocols to address systemic imbalances and prevent attack recurrence.
GV20 (Baihui) – Hundred Meetings
- Location: At the top of the head, at the midpoint of the line connecting the tops of the ears.
- Effects: Balances energy flow, calms the mind, and relieves headache pain. GV20 is a master point for neurological conditions and may influence hypothalamic function.
- Clinical Use: Used to enhance overall treatment efficacy and reduce attack frequency.
LR3 (Taichong) – Great Surge
- Location: On the foot, in the depression between the first and second toes.
- Effects: Soothes the liver meridian in TOM, which is associated with stress and emotional triggers. LR3 also reduces pain and promotes energy flow throughout the body.
- Clinical Use: Often needled to address stress-related attacks and improve systemic balance.

Treatment Protocol
- Point Selection: Acupuncturists typically combine 4–6 points per session, tailoring the selection to the patient’s symptoms (e.g., focusing on ST8 and GB20 for periorbital pain or PC6 for autonomic symptoms).
- Needling Technique: Needles are inserted to a depth of 0.5–1 inch, depending on the point, and left in place for 20–30 minutes. Gentle manual stimulation or electroacupuncture may enhance effects.
- Frequency: For acute cluster bouts, 1–2 sessions per week for 4–6 weeks are common. Chronic cases may require ongoing maintenance sessions (e.g., monthly).
- Adjunctive Techniques: Some practitioners use auricular (ear) acupuncture points, such as the trigeminal or shenmen points, to target headache pain and stress.
What to Expect During an Acupuncture Session
If you’re considering acupuncture for cluster headaches, here’s what to expect:
- Initial Consultation: The acupuncturist will review your headache history, triggers, and overall health to design a personalized treatment plan.
- Needle Insertion: Thin needles are inserted into selected acupoints. You may feel a slight pinch or tingling, but discomfort is minimal.
- Session Duration: Needles remain in place for 20–30 minutes while you relax. Some sessions include heat, moxibustion, or electroacupuncture.
- Frequency and Duration: Acute relief may require 1–2 sessions per week for 4–8 weeks. Chronic cases may need longer-term care.
- Safety: Acupuncture is safe when performed by a licensed practitioner. Minor side effects like bruising or soreness are rare.
Benefits of Acupuncture for Cluster Headaches
Acupuncture offers several advantages as a complementary therapy:
- Non-Invasive: No medications or invasive procedures, reducing the risk of side effects.
- Holistic Approach: Addresses physical pain, autonomic symptoms, and emotional triggers like stress.
- Complementary to Medications: Can be used alongside oxygen therapy or verapamil to enhance relief.
- Improved Quality of Life: May reduce attack frequency and improve sleep, mood, and coping ability.
Risks and Considerations
While acupuncture is generally safe, consider the following:
- Not a Cure: Acupuncture manages symptoms but does not eliminate cluster headaches.
- Practitioner Expertise: Choose a licensed acupuncturist with experience in headache disorders, certified by organizations like the National Certification Commission for Acupuncture and Oriental Medicine (NCCAOM).
- Cost and Access: Sessions cost $50–$150, and insurance coverage varies.
- Contraindications: Avoid acupuncture if you have a bleeding disorder, are pregnant (certain points are contraindicated), or have a pacemaker (if electroacupuncture is used).

Lifestyle Tips to Manage Cluster Headaches
In addition to acupuncture, these strategies can help:
- Avoid Triggers: Steer clear of alcohol, nicotine, and strong odors during cluster bouts.
- Maintain a Sleep Schedule: Go to bed and wake up at consistent times to stabilize circadian rhythms.
- Stress Management: Practice mindfulness, deep breathing, or yoga to reduce stress-related triggers.
- Track Symptoms: Keep a headache diary to identify patterns and triggers.
Conclusion
Cluster headaches are a devastating condition, but with the right treatment plan, relief is possible. Conventional therapies like oxygen and medications are effective for many, but acupuncture offers a promising complementary approach, particularly for those seeking natural, non-invasive options. By targeting key acupoints like GB20, LI4, and ST8, acupuncture can reduce pain, modulate neurological activity, and improve quality of life for cluster headache sufferers.
If you’re considering acupuncture, consult a licensed practitioner and work with your healthcare provider to integrate it into a comprehensive treatment plan. With acupuncture, lifestyle changes, and medical care, you can better manage cluster headaches and regain control over your life.
You need acupuncture treatment for Cluster headaches? Contact Fuji Wellness now!
Fuji Wellness:
- Address: 132-0031 Matsushima 1-chome, 21-14, Tokyo, Japan
- Chat with us: Click here
- Email: sunnyphamsensei@gmail.com







